This information will help you get ready for your endoscopic submucosal dissection (en-doh-SKAH-pik sub-myoo-KOH-sul dy-SEK-shun) procedure at MSK. Read this resource at least once before your procedure. Use it as a reference in the days leading up to your procedure.
What is an endoscopic submucosal dissection?
An ESD is a procedure to remove tumors in your digestive tract. Your digestive tract is made up of your esophagus (food pipe), stomach, small intestine, large intestine (colon), and rectum (see Figure 1).
A gastroenterologist (GAS-troh-EN-teh-RAH-loh-jist) will usually do your ESD during a colonoscopy (KOH-luh-NOS-koh-pee) or sigmoidoscopy (sig-MOY-DOS-koh-pee) procedure. A gastroenterologist is a doctor with special training in the gastrointestinal (GI) system. This includes the esophagus, stomach, and intestines.
Sometimes, the doctor cannot do an ESD during a colonoscopy or sigmoidoscopy. Talk with your healthcare provider about what to expect and how to get ready for your ESD. Follow the instructions in this resource carefully.
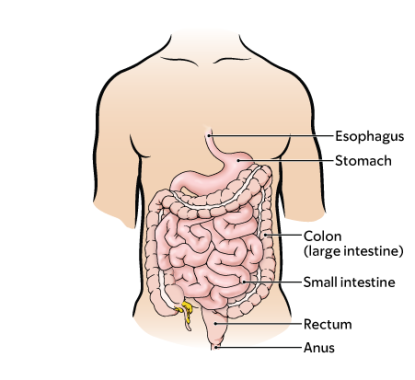
During your procedure, your doctor will place a flexible tube, called a colonoscope or sigmoidoscope, into your rectum. This will help them to see inside your anus, colon, and rectum (see Figure 1). The scope is connected to a video monitor. This allows them to see the inside of your colon.
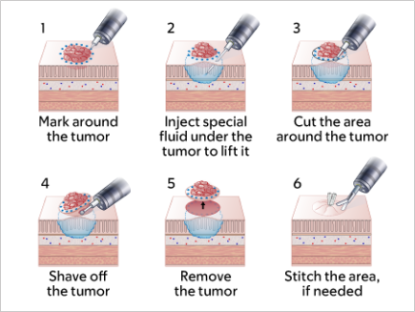
Your doctor will use air and fluid to move the scope along the length of your colon. They will do this while looking for anything that is not normal on the video monitor. They will use the scope to remove any tumors and stitch the area, if needed. When they’re finished, they will remove the scope.
Figure 2 shows the tumor removal process. The procedure usually takes 1 to 3 hours, but sometimes it may be longer.
What to do 2 weeks before your procedure
Ask about your medications
You may need to stop taking some of your medications before your procedure. Talk with your doctor about which medications are safe for you to stop taking. We have included some common examples below.
Do not stop taking any of your medications without talking with your doctor first.
Anticoagulants
If you take a blood thinner (medication that affects the way your blood clots), ask the doctor who prescribes it for you when you should stop taking it, and how many days until you need to start taking it again. Be sure to share this information with the doctor that will perform your ESD.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Medications for diabetes
If you take insulin or other medications for diabetes, you may need to change the dose. Ask the doctor who prescribes your diabetes medication what you should do the day before and the morning of your procedure.
If you take metformin (such as Glucophage® or Glumetza®) or a medication that contains metformin (such as Janumet®), do not take it the day before or the day of your procedure.
Get a letter from your doctor, if needed
A clearance letter is a letter from your doctor that says it’s safe for you to have a procedure. You may need to get one or more clearance letters before your procedure. Your MSK healthcare provider will tell you if you do. They must have your clearance letter at least 1 day before your procedure.
Clearance letter for an automatic implantable cardioverter-defibrillator (AICD) or permanent pacemaker (PPM)
Tell your MSK healthcare provider if you have an AICD or PPM. You will need a clearance letter from your cardiologist (heart doctor).
Clearance Letter for Other Symptoms
You’ll need a clearance letter from a doctor if you’ve had any of these during the last 6 weeks:
- Chest pain.
- Trouble breathing that’s new or has gotten worse.
- Fainting.
What to do 1 week before your procedure
Follow your healthcare provider’s instructions for taking aspirin
If you take aspirin, ask the doctor that prescribes it to you if you can stop taking it 1 week before your procedure. Aspirin and medications that contain aspirin can cause bleeding. Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil to learn more.
If your doctor doesn’t want you to stop taking aspirin, tell the doctor doing your ESD procedure at least 10 days before the procedure.
Arrange for someone to take you home
If your doctor cannot do an ESD during your procedure, you must have a responsible care partner take you home afterwards. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Buy supplies
- 4 (5 mg) tablets of bisacodyl (Dulcolax®). These are usually sold as a box of 10 tablets.
- 1 (238 gram) bottle of polyethylene glycol (MiraLAX ®).
-
64 ounces of any clear liquid that isn’t red, purple, or orange.
- A sports drink like Gatorade® or Powerade® is a good choice. Sports drinks will help replace electrolytes that you will lose during the bowel preparation (prep).
- If you have diabetes, be sure to get sugar-free clear liquids.
To see if you need any additional supplies, answer the questions below:
- Do you tend to be constipated? This can mean that you have fewer bowel movements (poop) than what’s usual for you, or have fewer than 3 bowel movements per week.
- Do you take narcotic (opioid) medications such as fentanyl (Duragesic®, Subsys®) morphine (DepoDur®, Duramorph, MS Contin®), hydrocodone (Vicodin®), or oxycodone (Oxycontin®, Percocet®)? If you’re not sure, ask your healthcare provider.
- Have you had a colonoscopy with a poor prep in the past?
If you answered yes to any of the questions, you must also buy the following supplies:
- 3 (17 gram) doses of MiraLAX (for a total of 51 grams). You can either buy 1 extra small bottle or the packets.
- Additional liquids for a full liquid diet. Read the “2 Days Before Your Procedure” section of this resource for examples of what you can drink.
What to do 5 days before your ESD procedure
5 days before your procedure
Stop taking iron supplements
If you take an iron supplement, stop taking it 5 days before your procedure. Iron supplements can cause color changes in your stool. This can make it harder for your doctor to see your colon clearly.
What to do 3 days before your procedure
Avoid certain foods
You should follow a low-fiber diet starting 3 days before your colonoscopy. During this time, do not eat:
- Raw (fresh) fruits and vegetables.
- Whole kernel corn, including canned corn.
- Whole grains, such as oatmeal, brown rice, quinoa, or wheat bread.
- Seeds, such as poppy or sesame.
- Nuts.
Talk with an endoscopy nurse
A few days before your procedure, you’ll get a phone call from an endoscopy nurse. They will review the instructions in this guide with you and ask you questions about your medical history. The nurse will also review your medications and tell you which to take the morning of your procedure.
What to do 2 days before your procedure
If you aren’t usually constipated, do not take narcotic (opioid) medications, or haven’t had a colonoscopy with poor prep in the past, you do not need to start your clear liquid diet until the day before your procedure. However, continue to avoid raw fruits and vegetables, beets (cooked or raw), red fruit juices, whole kernel corn, grains, seeds, and nuts. Skip to the next section “What to do the day before your procedure.”
If you’re usually constipated, take narcotic medications, or have had a colonoscopy with a poor prep in the past:
- Take 1 capful (17 grams) of MiraLAX mixed with 8 ounces of liquid at breakfast, lunch, and dinner.
-
Follow a full liquid diet, including:
- Yogurt without any pieces of fruit.
- Fruit juices without pulp.
- Soda.
- Broth or strained cream soups.
- Nutritional supplements such as Ensure® or Boost®.
- Ice cream and fruit ices without any pieces of fruit.
What to do the day before your procedure
Get your MiraLAX bowel prep ready
On the morning of the day before your procedure, mix all 238 grams of the MiraLAX powder with 64 ounces of a room temperature clear liquid until the MiraLAX powder dissolves. Once the MiraLAX is dissolved, you can put the mixture in the refrigerator. Many people find it tastes better chilled.
Do not mix the MiraLAX earlier than the morning of the day before your procedure.
Follow a clear liquid diet
You will need to follow a clear liquid diet the day before your procedure. Examples of clear liquids are listed in the table in this section.
- Do not eat any solid foods.
- Do not drink anything red, purple, or orange.
- Make sure to drink plenty of liquids in addition to water, coffee, and tea. This helps to make sure that you get enough calories and is an important part of your colonoscopy preparation. Try to drink at least 1 (8-ounce) glass every hour while you’re awake.
If you have diabetes, you should drink only sugar-free clear liquids and check your blood sugar level often. If you have any questions, talk with your healthcare provider.
| Clear Liquid Diet | ||
|---|---|---|
| Drink | Do Not Drink | |
| Soups |
|
|
| Sweets |
|
|
| Drinks |
|
|
Note the time of your procedure
A staff member will call you after noon (12 p.m.) the day before your procedure. If your procedure is scheduled for a Monday, they will call you on the Friday before. If you do not get a call by , call 212-639-5014, or the Admissions Office at 212-639-7882.
The staff member will tell you what time to get to the hospital for your procedure. They will also remind you where to go.
If you need to cancel your procedure, call the GI scheduling office at 212-639-5020.
Start your bowel prep
Bowel prep has 2 parts. Do part 1 of bowel prep the day before your procedure.
Part 1 of your bowel prep
At , swallow 2 Dulcolax tablets with a glass of water.
Drink 1 (8-ounce) cup of the MiraLAX mixture every 15 minutes at:
- 4:15 p.m.
- 4:30 p.m.
- 4:45 p.m.
- 5 p.m.
When you’re finished, half of the MiraLAX mixture will be left. Save the rest of it in the refrigerator for part 2 of your prep.
You should start having bowel movements within 1 hour of drinking part 1 of the MiraLAX mixture. This may take longer for some people.
Do not worry if you do not start having bowel movements after drinking part 1 of the MiraLAX. Keep drinking clear liquids to stay hydrated and flush out your colon.
After every bowel movement, put petroleum jelly (Vaseline®) or A & D® ointment on the skin around your anus. This helps prevent irritation caused by having loose stools and wiping often.
When you do part 2 depends on what time you were told to arrive for your procedure. If you were told to arrive before :
If you were told to arrive at or later:
|
Part 2 of your bowel prep (if you’re arriving before 11 a.m.)
Do not do this the night before your procedure if you are scheduled to arrive at or later.
At the night before your procedure, swallow 2 Dulcolax tablets with a glass of water.
Drink 1 (8-ounce) cup of the MiraLAX mixture every 15 minutes at:
- 11:15 p.m.
- 11:30 p.m.
- 11:45 p.m.
- 12 a.m. (midnight)
You should start having bowel movements within 1 hour after drinking part 2 of the MiraLAX mixture. If you don’t have bowel movements after 3 hours, call 212-639-2000. Ask to speak to the GI fellow on call.
You can drink clear liquids until 4 hours before your scheduled arrival time. Do not eat anything until after your procedure.
What to do the day of your procedure
Part 2 of your bowel prep (if you’re arriving at 11 a.m. or later)
At the morning of your procedure, swallow 2 Dulcolax tablets with a glass of water.
Drink 1 (8-ounce) cup of the MiraLAX mixture every 15 minutes at:
- 6:15 a.m.
- 6:30 a.m.
- 6:45 a.m.
- 7 a.m.
You should start having bowel movements within 1 hour after drinking part 2 of the MiraLAX mixture.
You can drink clear liquids until 4 hours before your scheduled arrival time. Do not eat anything until after your procedure.
Things to remember
- Take only the medications you were told to take the morning of your procedure. Take them with a few sips of water.
- Do not put any lotions, creams, or powder on your chest or arms.
- Remove any jewelry, including body piercings.
- Leave all valuables, such as credit cards and jewelry, at home. There won’t be lockers available to store your valuables in.
- If you wear contacts, wear your eyeglasses instead.
What to bring
- Your rescue inhaler (such as albuterol (Ventolin®) for asthma), if you have one.
- A case for your eyeglasses.
- Your Health Care Proxy form, if you have completed one.
- If you have an implanted pacemaker or cardioverter-defibrillator (AICD), bring your wallet card with you.
Where to go
Your procedure will take place at one of these locations:
David H. Koch Center
530 East 74th Street
New York, NY 10021
Take the elevator to the 8th floor.
Endoscopy Suite at Memorial Hospital (MSK’s main hospital)
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Surgery and Procedural Center through the glass doors.
Visit www.msk.org/parking for information about parking at these locations.
What to expect when you arrive
When it’s time for your procedure, a member of your care team will bring you into the procedure room. Your care team will attach equipment to monitor your heart, breathing, and blood pressure. You’ll get oxygen through a thin tube that rests below your nose. They’ll also place a mouth guard over your teeth to protect them.
Your nurse or anesthesiologist will place an intravenous (IV) line into a vein, usually in your arm or hand. You’ll get anesthesia through your IV, which will make you fall asleep. Once you’re asleep, your doctor will start the procedure.
Your procedure usually takes 1 to 3 hours, but sometimes it may be longer.
What to do after your procedure
Inside the Post-Anesthesia Care Unit (PACU)
When you wake up, you’ll be in the PACU. Your nurse will continue to monitor your heart, breathing, and blood pressure.
If your doctor did an ESD, you’ll need to stay in the hospital overnight so your nurse can monitor you. You’ll move to an inpatient bed when one is available. If you do not have any issues overnight, you’ll be able to leave the hospital the next day.
If your doctor did not do an ESD, you can go home the same day. You must have a responsible care partner take you home afterwards.
At home
For the first 7 days after your procedure:
- Do not drink alcohol.
- Do not do any strenuous exercise (such as jogging and tennis).
- Do not lift anything heavier than 10 pounds (4.5 kilograms).
- Try to stay local, and do not travel long distances, such as outside of the country.
It’s normal for your bowel movements to be irregular or different from your usual habits. This may last for up to a week after your procedure.
It’s normal to have a small amount of bleeding from your rectum. There should be no more than a few drops of blood, and the bleeding should stop within 24 hours after your procedure.
Most people can go back to work 7 days after having this procedure, but everyone is different, so it may be shorter or longer for you. If you need to do a lot of heavy lifting at your job, talk with your doctor before going back to work.
Follow-up care
You’ll have a follow-up visit with your healthcare provider 2 weeks after your procedure. During this visit, they will talk with you about your results and go over a treatment plan.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Intense pain, hardness, or swelling in your abdomen (belly).
- Blood in your vomit (throw up).
- Bleeding from your anus for more than 24 hours.
- Weakness, faintness, or both.
- Any other questions or concerns.
If you have chest pain or trouble breathing, call 911 or go to your nearest emergency room.
Contact information
If you have any questions or concerns, call Dr. Nishimura’s office at 212-639-6029, or Dr. Beauvais’ office at 212-639-5909. You can reach a staff member Monday through Friday from to After , during the weekend, and on holidays, call 212-639-2000 and ask for the GI doctor on call.