This information explains what a PICC is and how it’s placed. It also has guidelines for caring for your PICC at home. A PICC is a type of central venous catheter (CVC).
What is a PICC?
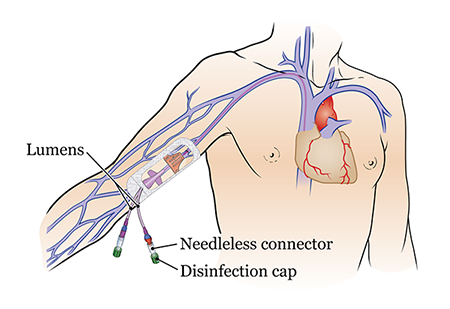
A PICC is a long, flexible catheter (thin tube) that goes into a vein in your upper arm. The PICC goes through the vein in your arm to a large vein in your chest.
Outside your body, the PICC splits into 1, 2, or 3 smaller tubes called lumens. Each lumen has a needleless connector (also called a clave) and a disinfection cap on the end (see Figure 1).
What is a PICC Used For?
A PICC lets your care team put liquids into your bloodstream and take blood samples more easily. Having a PICC means they will not need to put needles in your body as often. This can make your treatment more comfortable.
Your care team can use your PICC to:
- Give you chemotherapy and other intravenous (IV) medications, such as antibiotics.
- Give you blood transfusions.
- Give you IV fluids.
- Take blood samples.
Some PICCs can also be used to put contrast dye into your bloodstream. You might get contrast dye before medical imaging tests, such as before a computed tomography (CT) scan. Contrast makes differences inside your body easier to see.
How long can you have a PICC?
A PICC can stay in your body for as long as you need it for your treatment. Your healthcare provider will take it out when you don’t need it anymore.
Having a PICC should not keep you from doing most of your day-to-day activities. You will still be able to go to work or school.
It’s important that the dressing over your PICC stays clean, dry, and unbroken.
While you have a PICC, do not:
- Do any activities that make you sweat.
- Swim or go in a hot tub.
- Play contact sports, such as football and soccer.
- Move the arm with your PICC in a repetitive motion (the same motion over and over). Vacuuming, golfing, push-ups, and biceps curls are examples of repetitive motions.
- Carry objects heavier than 5 to 10 pounds (2.3 to 4.5 kilograms) with the arm with your PICC.
It’s OK to do low-energy, low-movement activities, such as walking or stretching.
Before the procedure to place your PICC
Your nurse will tell you how to get ready for your procedure. They’ll also teach you how to care for your PICC after your procedure. You can have a caregiver, family member, or friend learn with you.
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
Take devices off your skin
You may wear certain devices on your skin. Before your scan or procedure, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
Talk with your healthcare provider about scheduling your appointment closer to the date you need to change your device. Make sure you have an extra device with you to put on after your scan or procedure.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
Tell us if you’re sick
If you get sick before your surgery, call the healthcare provider who scheduled your surgery. This includes a fever, cold, sore throat, or the flu.
You can reach them Monday through Friday from to After , during the weekend, and on holidays, call 212-639-2000. Ask for the doctor or nurse on call.
The day of the procedure to place your PICC
On the day of your procedure:
- You can eat and drink like usual.
- You can take your usual medications.
- Do not put cream (thick moisturizers) or petroleum jelly (Vaseline®) on your skin.
Once you get to the hospital, many staff members will ask you to say and spell your name and date of birth. This is for your safety. People with the same or a similar name may be having a procedure on the same day.
What to expect during the procedure to place your PICC
A doctor or nurse will place your PICC. The procedure will take about 30 to 45 minutes.
First, you’ll get a numbing injection (shot) of lidocaine in your arm where your PICC will be placed. Tell the doctor or nurse if you’re allergic to lidocaine or nickel before they give you the shot.
If you have your PICC placed in Interventional Radiology, they may give you sedation (seh-DAY-shun). Sedation is when you’re calm, relaxed, or sleepy from medicine you get before your injection.
Once the area is numb, the doctor or nurse will use a needle to put the PICC into your vein. They’ll use an ultrasound scan to help them see your vein. They will also use the ultrasound to check the PICC is OK to use once it’s in place. You may also need a chest X-ray to check the PICC is OK to use.
Once the PICC is in place, the doctor or nurse will cover the part outside your body. This will keep it from moving. They will either use a SecurAcath® (see Figure 2) or StatLock® (see Figure 3). They will also put StatSeal® over the insertion site to prevent any bleeding or oozing.
.
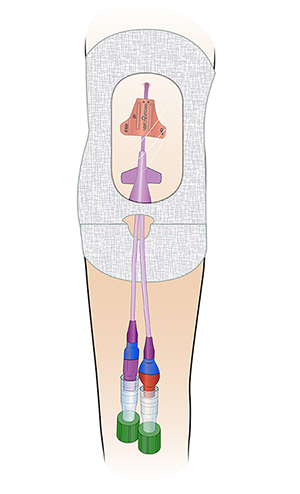
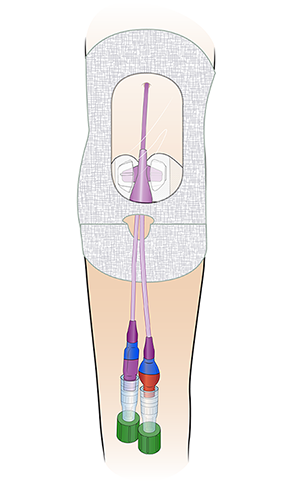
If you have a SecurAcath, it will stay in place the whole time you have the PICC. If you have a StatLock, you will need to have a nurse change it every time they change your dressing.
Once your PICC is secure, the doctor or nurse will put a Tegaderm™ dressing over the exit site. The exit site is the place where your PICC leaves your body. This will keep it clean. You’ll need to have your dressing changed weekly, or whenever it’s dirty, wet, or torn. Keep the dressing clean, dry, and secure.
If your PICC gets pulled out, you’ll need to have it replaced.
Your care team will remove your PICC after your treatment is finished. They may also remove it if there is something wrong with the line, such as:
- A line infection.
- Leaking or cracks in the line.
- Your care team cannot flush one of the lumens.
After the procedure to place your PICC
If you had your PICC placed in Interventional Radiology with sedation, your care team will monitor you after the procedure. A nurse will keep track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth.
You’ll stay in bed until the sedation wears off. Then, you’ll go back to your hospital room or get discharged from the hospital.
Your arm may feel heavy until the effects of the lidocaine wear off. The insertion site may feel a little sore. You may also have some mild discomfort at your catheter exit site. This can last for about 1 to 3 days after your PICC is placed.
If you have any bleeding from your exit site, apply pressure and a cold compress to the area. Blood can be a source of infection. If blood collects beneath your dressing, call your care team to schedule an appointment to have your dressing changed.
Call your doctor or nurse if the bleeding and discomfort gets worse at any time.
Do not shower for 24 hours after your procedure.
Your discharge kit
Your nurse will give you an emergency kit before your procedure or before you’re discharged from the hospital.
The emergency kit has:
- 1 toothless clamp.
- 2 face masks.
- 1 alcohol-based (Purell®) hand wipe.
- 1 disposable drape.
- 2 pairs of sterile gloves.
- Alcohol pads.
- 1 needleless connector.
- 2 Tegaderm CHG dressings.
- Waterproof covers.
- Disinfection caps.
- Your doctor’s office and emergency telephone numbers.
Keep this kit with you at all times. You’ll need it if:
- Your PICC is leaking.
- Your Tegaderm dressing is damaged or comes off.
- Your needleless connector or disinfection cap falls off.
How to care for your PICC at home
Ask your nurse about the best way to secure your catheter. Do not put tape over the connection site. This is where the needleless connector connects to the lumens.
Check your exit site every day for:
- Redness
- Tenderness
- Leakage
- Swelling
- Bleeding
If you have any of these signs or symptoms, call your doctor. You may have an infection.
Do not have any of the following on the arm where your PICC was placed:
- Needle sticks, such as for blood draws or an IV line.
- Blood pressure measurements.
- Tight clothing or tourniquets.
At least once a week, you’ll need to have these changed:
- Tegaderm dressing. Do not change your Tegaderm dressing yourself.
- Needleless connectors.
- Disinfection caps.
You must have your PICC flushed once a week. A nurse should flush your PICC. If you’re going home with your PICC, your care team may teach you or a family member how to flush the lumens.
It’s best if you can come to a MSK location so a nurse can care for your PICC. If you cannot come to an MSK site, your nurse will help you make other arrangements. Always contact your doctor or nurse if you have any questions.
What to do if your PICC is leaking
- Clamp your PICC line above the leak. Use the clamp in your discharge kit.
- Wipe the area that’s leaking with an alcohol pad.
- Call your doctor or nurse right away.
If fluid is leaking while you’re getting an infusion, check that the needleless connector is on tightly. If it’s still leaking, call your doctor or nurse right away.
If you’re getting an infusion at home and fluid is leaking from your exit site, turn off the infusion. Call your doctor or nurse right away.
What to do if your Tegaderm dressing is damaged, loose, or dirty
Put a new Tegaderm dressing over the damaged, loose, or dirty dressing. Do not take off the damaged, loose, or dirty dressing.
Call your doctor or nurse right away.
What to do if your Tegaderm dressing is wet
Call your doctor or nurse right away. Do not take off the wet Tegaderm dressing or put another dressing over it.
What to do if your disinfection cap falls off
Throw the disinfection cap that fell off in the trash. Do not put it back on the lumen.
To put on a new disinfection cap:
- Clean your hands with soap and water or an alcohol-based hand sanitizer.
- Get a new disinfection cap from your discharge kit. Take the cap off the strip.
- Hold the needleless connector in one hand. With your other hand, gently push and twist the new disinfection cap onto the end of the needleless connector.
What to do if your needleless connector falls off
Throw the needleless connector that fell off in the trash. Do not put it back on the lumen.
To put on a new needleless connector:
-
Gather your supplies. You’ll need:
- 1 pair of medical gloves
- 2 alcohol pads
- 1 new needleless connector
- 1 new disinfection cap
- Clean your hands with soap and water or an alcohol-based hand sanitizer. Put the gloves on.
-
Get your supplies ready.
- Open 1 of the alcohol pad packets, but leave the alcohol pad inside.
- Open the needleless connector packet, but leave the needleless connector inside.
- Pull the tab to take the cover off the disinfection cap. Leave the disinfection cap inside its plastic holder.
-
Open the other alcohol pad packet. Using the alcohol pad inside, pick up the lumen with your non-dominant hand. This is the hand you do not write with. Hold the lumen close to the end (see Figure 4).
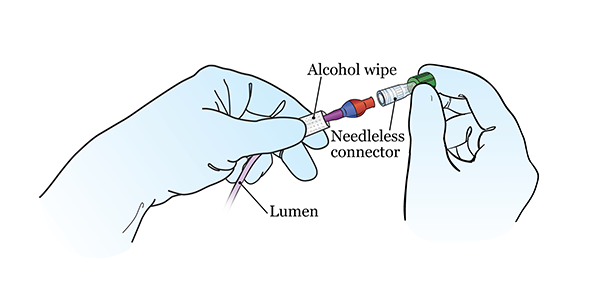
Figure 4. Twisting a new needleless connector onto the lumen - Pick up the other alcohol pad with your dominant hand. This is the hand you write with. Scrub the open end of the lumen with the alcohol pad for 15 seconds. Then throw the alcohol pad in the trash. Let the lumen dry for 15 seconds. Keep holding it with the alcohol pad in your non-dominant hand.
- Pick up the new needleless connector with your free hand. If it has a cover, take the cover off. You can do this using the knuckles of your other hand.
- Twist the new needleless connector onto the end of the lumen (see Figure 4). Keep holding the lumen with the alcohol pad in your non-dominant hand.
- With your free hand, pick up the plastic holder with the disinfection cap. Gently push and twist the disinfection cap onto the end of the needleless connector. Once it’s attached, pull off the plastic holder and throw it away.
- Take your gloves off. Clean your hands.
Call your doctor or nurse after you change the needleless connector.
How to shower with a PICC
Follow the instructions in this section when you shower. Do not submerge your PICC in water (such as in a bathtub or swimming pool). Watch Showering While You Have a Central Venous Catheter (CVC) to learn more about showering with a PICC.
Use a waterproof cover
You can shower with your PICC in place. Use a single-use waterproof cover, such as Aquaguard®. This goes over your dressing to keep it from getting wet. You can buy waterproof covers online.
Each time you shower, cover your Tegaderm dressing completely with a new waterproof cover. To put on the cover:
- Peel off the top and side strips.
- Place the top edge above your dressing. Do not let the tape on the waterproof cover touch your Tegaderm dressing. It can lift your dressing when you remove the waterproof cover after showering. Smooth the cover down over your dressing.
- Peel off the bottom strip. Make sure the bottom edge of the waterproof cover is below your dressing. Make sure the lumens of your PICC are tucked into the waterproof cover and completely covered. Smooth the bottom edge down.
Do not shower for longer than 15 minutes. Use warm water, not hot water. This will help keep the waterproof cover from coming off.
After your shower, dry the waterproof cover before removing it.
Use a 4% chlorhexidine gluconate (CHG) solution antiseptic skin cleanser (such as Hibiclens®)
It’s important to keep your skin clean while your PICC is in place. Showering with a 4% CHG solution will help lower your risk of infection.
Wash with a 4% CHG solution antiseptic skin cleanser every day while your PICC is in place. An antiseptic is something that kills bacteria and other germs. 4% CHG solution is an antiseptic that kills germs for up to 24 hours after you use it.
You can buy a 4% CHG solution antiseptic skin cleanser from any local pharmacy or online. A staff member will also give you a small bottle when you’re discharged from the hospital.
Instructions for using a 4% CHG solution antiseptic skin cleanser
- Wash your hair with your usual shampoo and conditioner. Rinse your head well.
- Wash your face and genital (groin) area with your usual soap. Rinse your body well with warm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Do not put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne after your shower.
Important points to remember when using 4% CHG solution
- Do not use regular soap, lotion, cream, powder, or deodorant without talking with your nurse first. If you’re in the hospital, your nurse may give you lotion that you can use after using 4% CHG solution.
- Do not use 4% CHG solution on your head, face, ears, eyes, mouth, genital area, or on deep wounds. If you have a wound and are not sure if you should use 4% CHG solution on it, ask your doctor or nurse.
- Do not use 4% CHG solution if you’re allergic to chlorhexidine.
- If your skin gets irritated or you have an allergic reaction when using 4% CHG solution, stop using it. Call your doctor.
When to call your healthcare provider
Call your healthcare provider right away if you:
- Pull your PICC line out of place or think you might have pulled it out of place.
- Have a fever of 100.4 °F (38 °C) or higher.
- Have shortness of breath.
- Feel lightheaded or dizzy.
- Feel nauseous (feeling like you’re going to throw up) or vomiting (throwing up).
- Feel confused.
- Have discomfort in your chest.
- Have swelling in your hand, fingers, upper arm, neck, or at your exit site.
- Have aching in the arm where your PICC is placed.
- Have heart palpitations (a faster heartbeat than usual).
- Have numbness or tingling in your arm, hands, or fingers of the arm where the PICC line is placed.
- Have bleeding from the PICC line site or exit site.
- Have redness or warmth at the PICC line site or in the arm with the PICC line
- Have redness at your exit site.
- Have leakage from your PICC line or exit site.
- Feel tenderness at your exit site.
