This information will help you get ready for your pleuroscopy (ploor-OS-koh-pee) at MSK. It also explains what to expect before, during, and after your procedure.
About your pleuroscopy
A pleuroscopy is sometimes called a medical thoracoscopy (THOR-uh-KOS-koh-pee). A pleuroscopy is a procedure that lets your doctor look inside your pleural cavity. Your pleural cavity is the space between your chest wall and lung (see Figure 1).
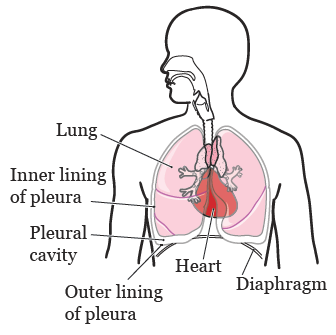
Your doctor will use a pleuroscope (PLOOR-oh-SKOPE) to look inside your pleural cavity. A pleuroscope is a thin tube with a light and camera on the end of it. During your pleuroscopy, your doctor will put the pleuroscope through your chest wall, into your pleural cavity.
Once the pleuroscope is in your pleural cavity, your doctor will do 1 or more of these things:
- Do a biopsy (take small tissue samples).
- Drain fluid from your pleural cavity.
- Put medication into your pleural cavity to keep fluid from building up. This is called pleurodesis (PLOOR-oh-DEE-sis).
- Place a PleurX™ catheter (a thin, flexible tube) through your chest wall. This will help drain fluid from your pleural cavity after your procedure.
Your healthcare provider will give you information and talk with you about what to expect during your procedure.
What to do before your pleuroscopy
Talk with a nurse and plan your care
Before your procedure, you’ll talk with a nurse to plan your care during your procedure. The way you talk with the nurse depends on where your procedure will be done. Your healthcare provider will tell you what to expect.
Presurgical testing (PST)
Your healthcare provider will tell you if you need presurgical testing (PST) before your procedure. PST is a regular physical exam. It can also include other medical tests that will give your care team important information about your health. PST helps your care team find out if you’re healthy enough to have the procedure.
If you need PST, you will be scheduled for an appointment within 30 days (1 month) of your procedure. The date, time, and location will be printed on the appointment reminder from your healthcare provider’s office. You can eat and take your usual medications the day of your appointment.
It’s helpful to bring these things to your PST appointment:
- A list of all the medications you’re taking, including prescription and over-the-counter medications, patches, and creams.
- Results of any tests done outside of MSK, such as a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
During your PST appointment, you’ll meet with a nurse practitioner (NP). They work closely with anesthesiology staff (specialized healthcare providers who will give you anesthesia during your procedure). Your NP will review your medical and surgical history with you. You may also have medical tests to help plan your procedure, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your NP may recommend you see other healthcare providers. They will also talk with you about which medications to take the morning of your procedure.
Getting ready for your procedure
You and your care team will work together to get ready for your procedure. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
You may need to follow special instructions before your procedure based on the medicines and supplements you take. If you do not follow those instructions, your procedure may be delayed or canceled.
-
I take any prescription medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. Examples include:
- Medicines you swallow.
- Medicines you take as an injection (shot).
- Medicines you inhale (breathe in).
- Medicines you put on your skin as a patch or cream.
- I take any over-the-counter medicines, including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take any dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to make you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I use recreational drugs, such as marijuana.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your procedure. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medications to help prevent them.
Here are things you can do before your procedure to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
-
Try to stop drinking alcohol once your procedure is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and procedures. All your medical information will be kept private, as always.
About smoking
If you smoke or use an electronic smoking device, you can have breathing problems when you have a procedure. Vapes and e-cigarettes are examples of electronic smoking devices. Stopping for even a few days before your procedure can help prevent breathing problems during and after your procedure.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Blood thinners
Blood thinners are medications that affect the way your blood clots. If you take blood thinners, ask the healthcare provider performing your procedure what to do. They may recommend you stop taking the medication. This will depend on the type of procedure you’re having and the reason you’re taking blood thinners.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Diabetes medicines
If you take insulin or other diabetes medicines, talk with the healthcare provider doing your procedure and the healthcare provider who prescribes it. Ask them what to do before your procedure. You may need to stop taking it or take a different dose (amount) than usual. You may also need to follow different eating and drinking instructions before your procedure. Follow your healthcare provider’s instructions.
Your care team will check your blood sugar levels during your procedure.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Diuretics (water pills)
A diuretic is a medicine that helps control fluid buildup in your body. Diuretics are often prescribed to help treat hypertension (high blood pressure) or edema (swelling). They can also be prescribed to help treat certain heart or kidney problems.
If you take a diuretic, ask the healthcare provider doing your procedure what to do before your procedure. You may need to stop taking it the day of your procedure.
We’ve listed some examples of common diuretics below. There are others, so be sure your care team knows all the medicines you take.
|
|
Learn how to care for your PleurX catheter, if needed
If you’re having a PleurX catheter placed, your nurse will show you how to care for it before your procedure. For more information, read About Your PleurX™ Catheter.
Get a letter from your doctor, if needed
If you have an automatic implantable cardioverter-defibrillator (AICD), talk with your cardiologist (heart doctor) about your procedure. You may need to get a clearance letter from them before your procedure. A clearance letter is a letter that says you can have the procedure. Follow your care team’s instructions.
Arrange for someone to take you home, if needed
If you’ll be discharged (leaving the hospital) the same day as your procedure, you must have a responsible care partner take you home. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They will send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do the day before your pleuroscopy
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
What to do the day of your pleuroscopy
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Follow your healthcare provider’s instructions for taking your medications the morning of your procedure. It’s OK to take them with a few small sips of water.
- Wear loose, comfortable clothing.
- If you wear contact lenses, wear your glasses instead, if you can. If you don’t have glasses, bring a case for your contacts.
- Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Take off any jewelry, including body piercings.
- Leave valuable items, such as credit cards and jewelry, at home.
- When it’s time for your procedure, you’ll need to remove your hearing aid(s), dentures, prosthetic device(s), wig, and religious articles.
What to bring
- A list of all the medications you take at home, including patches and creams.
- Your rescue inhaler (such as albuterol for asthma), if you have one, or any other medications for breathing.
- Your cell phone and charger.
- Only the money you may want for small purchases, such as a newspaper.
- A case for your personal items, if you have one. This includes glasses or contacts, hearing aid(s), dentures, prosthetic device(s), wig, or religious articles.
- Your Health Care Proxy form and other advance directives, if you have filled them out.
- Your breathing device for sleep apnea (such as your CPAP machine), if you use one. If you can’t bring it, we will give you one to use while you’re in the hospital.
- If you have an implanted pacemaker or automatic implantable cardioverter-defibrillator (AICD), bring your wallet card with you.
Where to go
Your procedure will be done at:
Endoscopy suite at Memorial Hospital (the main hospital at MSK)
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Surgery and Procedural Center through the glass doors.
For information about MSK’s locations, including directions and parking options, visit www.msk.org/locations
What to expect when you arrive at the hospital
Many doctors, nurses, and other staff members will ask you to state and spell your name and date of birth. This is for your safety. People with the same or similar names may be having procedures on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown and nonskid socks to wear. You’ll be asked to remove your glasses or contacts, hearing aid(s), dentures, prosthetic device(s), wig, or religious articles, if you have any.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicine, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
The IV will be used to give you anesthesia (medication to make you sleepy) during your procedure. You may also get fluids through the IV before your procedure.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Meet with your doctor
You’ll talk with your doctor before your procedure. They will explain the procedure and answer your questions.
What to expect during your pleuroscopy
When it’s time for your procedure, you’ll go into the procedure room and be helped onto an exam table. You’ll lie on your side with your arm extended. Your healthcare provider will set up equipment to monitor your heart rate, breathing, and blood pressure. You’ll also get oxygen through a thin tube that rests below your nose.
Once you’re in the right position, your doctor will use an ultrasound machine to look at your chest. An ultrasound is an imaging test that uses sound waves to make pictures of the inside of your body. Your doctor will use the ultrasound to choose the best place to make the incisions (surgical cuts) for your procedure.
Then, you’ll get anesthesia through your IV line. Once you’re sleepy, your doctor will make 1 to 2 incisions in your chest (see Figure 2). One incision will be for the pleuroscope. The other will be for the surgical tools your doctor will use during your procedure, if needed. You will not feel your doctor make the incisions.
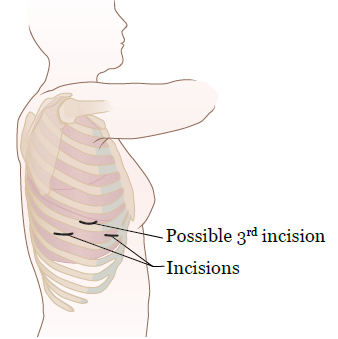
Once the pleuroscope is in your pleural cavity, your doctor may do a biopsy, drain fluid, or do a pleurodesis. They may do all 3 things.
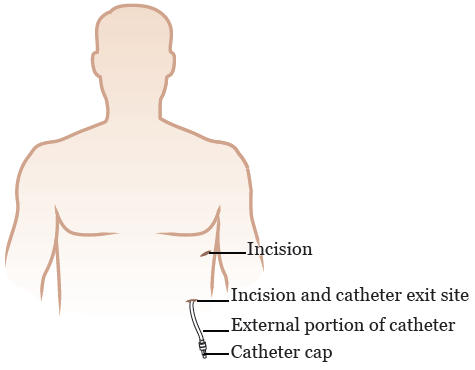
If you’re having a PleurX catheter placed, your doctor will make 1 or 2 more small incisions in your chest. One incision is for the catheter to go into your pleural cavity. Your doctor may be able to use an incision they already made for this. The other incision is for the catheter to leave your body. This is called the catheter exit site. It will be a few inches away from the incision into your pleural cavity.
Once the incisions are ready, your doctor will place your PleurX catheter. It will go into your pleural cavity, under your skin, then out of your body (see Figure 3). Tunneling the catheter under your skin helps the catheter stay in place.
The pleuroscopy usually takes about 40 to 60 minutes.
What to expect after your pleuroscopy
In the post-anesthesia care unit (PACU)
When you wake up after your procedure, you’ll be in the Post-Anesthesia Care Unit (PACU).
A nurse will keep track of your body temperature, pulse, blood pressure, and oxygen levels. You’ll have a chest X-ray to make sure your lung was not damaged. This type of injury is rare.
You’ll have a chest tube to drain air and fluid out of your pleural cavity. You may also have a PleurX catheter. You may have some discomfort at your chest tube or PleurX catheter exit site. If you do, ask your nurse for medication to help ease your pain.
Depending on the type of procedure you had, you may be admitted to the hospital for a few days. If you don’t need to stay in the hospital, you’ll be discharged the same day as your procedure.
If you’re admitted to the hospital
If you’re staying in the hospital after your procedure, you’ll be moved from the PACU to a hospital room. While you’re in the hospital, your care team will keep track of the drainage coming from your pleural cavity.
Your chest tube will stay in place while you’re in the hospital. It will be taken out once there’s no more air or fluid draining from your pleural cavity. It can also be taken out when the amount of drainage is low enough.
After your chest tube is taken out, the site will be closed with sutures (stitches) and covered with a bandage. Keep the bandage on for at least 48 hours (2 days) unless your healthcare provider gives you other instructions.
How long you stay in the hospital depends on many things. You may need to stay in the hospital longer because you have:
- Air leaking from your lung.
- A fever of 101 °F (38.3 °C) or higher, or other signs of an infection.
- Subcutaneous emphysema (SUB-kyoo-TAY-nee-us EMP-fuh-ZEE-muh). This is when air is trapped under your skin.
- Bleeding.
- High fluid output (a large amount of fluid draining from your pleural cavity).
If you have a PleurX catheter, it will still be in place when you leave the hospital. A nurse will show you how to care for it before you’re discharged. For more information, read About Your PleurX™ Catheter.
If you’re discharged the same day as your procedure
If you’re being discharged the same day as your procedure, your chest tube will be taken out while you’re in the PACU. You’ll be discharged once you’re fully awake and your pain is managed.
If you have a PleurX catheter, it will still be in place when you leave the hospital. A nurse will show you how to care for it before you’re discharged. For more information, read About Your PleurX™ Catheter.
You must have a responsible care partner take you home. Read the section “Arrange for someone to take you home, if needed” for more information.
What to do after you leave the hospital
You may have some discomfort at your PleurX catheter exit site. This usually goes away within a few hours of your procedure. If you still have pain or discomfort after taking pain medication, call your healthcare provider’s office.
Caring for your incisions
You’ll have 1 to 2 incisions that are closed with sutures and covered with a bandage. If you have a PleurX catheter, you’ll also have 1 incision for it.
- The bandage over the sutures can be taken off after 48 hours (2 days), only if there’s no fluid draining from the incision. If there’s fluid draining, put gauze over your incision, then cover it with a bandage. If fluid keeps draining for longer than 3 days, call your healthcare provider’s office.
- You can shower once the bandage is off. Every time you shower, cover your PleurX catheter with a one-time-use waterproof cover, such as AquaGuard®. You can buy waterproof covers online. Do not take tub baths or swim while you have your catheter.
- Your sutures will be taken out at your next follow-up appointment in 2 to 4 weeks.
Call your healthcare provider’s office if you notice any redness, swelling, or pus-like (thick or milky) drainage from your incision. These things can be signs of infection.
Draining your PleurX catheter
For information about draining your PleurX catheter, read About Your PleurX™ Catheter. If you have any questions, call your healthcare provider’s office.
Lifting heavy objects
Check with your doctor before you do any heavy lifting. Most people should not lift anything heavier than 10 pounds (4.5 kilograms) for at least 3 weeks after their procedure. Ask your doctor how long you should avoid heavy lifting.
Exercising
The best kind of exercise to do after your procedure is aerobic (ayr-OH-bik) exercise. Aerobic exercise is any exercise that makes your heart beat faster, such as walking or climbing stairs. Do this kind of exercise for at least 30 minutes each day.
You can start exercising again right after your procedure unless your doctor gives you other instructions. Remember, it will take time to get back to the activity level you were at before your procedure. Start out slowly and increase your activity level as you feel better.
Do not do any kind of heavy exercise or play contact sports until your doctor tells you it’s safe. Examples of contact sports are football, soccer, and basketball.
Follow-up appointment
You’ll have a follow-up appointment with your doctor 2 to 4 weeks after your procedure. Your sutures will be taken out then.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Trouble breathing or shortness of breath.
- Chest pain or a feeling of pressure in your chest.
- Pain, redness, or swelling at your incision site(s) that’s getting worse.
- Fluid draining from your incision site(s) for more than 3 days.
- Pus-like (thick or milky) drainage from your incision site(s).
- Trouble draining your PleurX catheter.
- Pain or discomfort, even after taking pain medication to help.