Watch How Two MSK Labs Came Together to Give a Stage 4 Lung Cancer Patient More Time
For more than a decade, MSK neuro-oncologist Adrienne Boire, MD, PhD, has been studying leptomeningeal metastases (LM), a devastating complication where cancer spreads to the cerebrospinal fluid surrounding the brain and spinal cord.
Now Dr. Boire’s years of painstaking work and close collaboration with a computational biologist have led to a clinical trial testing a new treatment for LM. The phase 1 trial involves giving a drug called deferoxamine (DFO) by intrathecal injection directly into the cerebrospinal fluid. It’s the first trial to test the drug in this way, and several patients have survived months — in some cases a year — longer than expected. This potential treatment for leptomeningeal metastases is not a cure, but it is giving patients more precious time.
“I’ve always dreamt that someday I would be able to find something in my laboratory that would make a meaningful difference in someone’s life,” Dr. Boire says. “This is the first laboratory focused on the study of leptomeningeal metastasis. It’s the sort of problem no one person can solve.”
Dr. Boire teamed with computational biologist Dana Pe’er, PhD, to identify the trick that cancer cells use to survive and grow in the spinal fluid. By conducting a detailed analysis of patient samples using powerful computational methods, they unearthed the secret — a discovery that also suggested a treatment strategy.
“This is the soul of science,” Dr. Boire says. “Everyone is working together to understand different parts of the same problem. We find and create something that could never have been seen before.”
Lab Research Leads to Clinical Trial for Leptomeningeal Metastasis
Although rare, LM is becoming more common as people live longer with stage 4 cancer. About 5% to 10% of cancer patients now develop leptomeningeal metastasis, and, even with treatment, the median survival is three to four months. The symptoms of LM include pain, seizures, difficulty thinking, and a loss of muscle control. There is no cure or effective therapy.
Dr. Boire first set out to crack the mystery of LM in 2014. Frustrated by the lack of effective therapies for her patients, she focused her research on how cancer cells spread and manage to survive in the leptomeningeal space, which typically lacks nutrients.

There isn’t much fuel for cells around the brain and spinal cord because they are largely sealed off from the rest of the body by the blood-brain barrier, a network of blood vessels and tissue with tightly packed cells. To better understand the fundamental biology at work, Dr. Boire and colleagues in the lab of Joan Massagué, PhD, began studying human LM cells in mice. They found that a protein called C3 opens the membrane between the blood and spinal fluid and allows growth factors and nutrients from the blood to enter and sustain the cancer cells.
This discovery, however, did not fully explain how LM cells survived in the mostly barren environment. Immune cells also invade the spinal fluid and vastly outnumber the cancer cells, competing for the same nutrients. Even so, some of the cancer cells survive.
Analyzing Cancer, One Cell at a Time
To find out how the cancer cells get what they need, Dr. Boire teamed with Dr. Pe’er, a world-renowned expert in single-cell analysis — which studies cancer and its ecosystem one cell at a time. This new technology enables scientists to understand which genes are active in each cell.
One of the main tools of single cell analytics is called single-cell RNA-seq, which looks at RNA rather than DNA. (RNA is the messenger that carries instructions from DNA to build proteins and perform vital functions). Using RNA-seq, investigators can determine which genes are expressed, or “turned on,” in cells. Because every cell in the body contains the same DNA, RNA analysis provides much-needed detail about cell function and activity.
“Dr. Boire came to me and said, ‘Maybe this technology can help me figure out how to help my patients,’” Dr. Pe’er recalls. “Nothing made me happier — I came to MSK to use my math skills to help people — and I said, ‘Yes, let’s do this.’”
It was slow going at first. Dr. Pe’er found the leptomeningeal space an “alien, weird environment” that was much different from any she had studied before. Her team had spent years developing computational tools to interpret such data, but these failed out of the box. Eventually, her team adapted the tools to detect patterns in the RNA expression that would show the scientists how the cancer cells were surviving.
“Less than a decade ago, it would have been unimaginable to do what our RNA-seq machine can do,” Dr. Pe’er says. “We have the technology now to measure and computationally analyze billions of data points to identify patterns that reveal what is going on in the cells.”
How LM Cells Overtake Immune Cells
The researchers found that LM cells reprogram themselves to produce a protein called lipocalin-2. This protein binds to iron, which LM cells need to survive.
Dr. Boire’s team showed that increased lipocalin-2 levels enable the cancer cells to monopolize the iron and outcompete the immune cells. It’s like the LM cells are creating a much stronger magnet to pick up more paper clips.

Based on this discovery, Dr. Boire had an idea about how to stop the cancer cells. In mice, Dr. Boire delivered chemical compounds called iron chelators directly into the spinal fluid. The theory was that the chelators would bind to the iron, making less of it available to all the cells and taking away the cancer cells’ advantage. Dr. Boire’s hypothesis proved to be true.
“It reminds me of when kids are fighting over a toy, and the parent says, ‘That’s it — I’m taking it away. Nobody gets it,’ ” Dr. Boire says.
Based on this finding, she launched a clinical trial in 2021 testing whether the iron chelator drug deferoxamine (DFO) could be safe and effective in treating LM in cancer patients. Patients receive DFO through a small plastic tube called an Ommaya reservoir, which allows the drug to be inserted directly into the brain’s ventricle, bypassing the blood-brain barrier.
Treatment Stops LM for Patient Given Months to Live
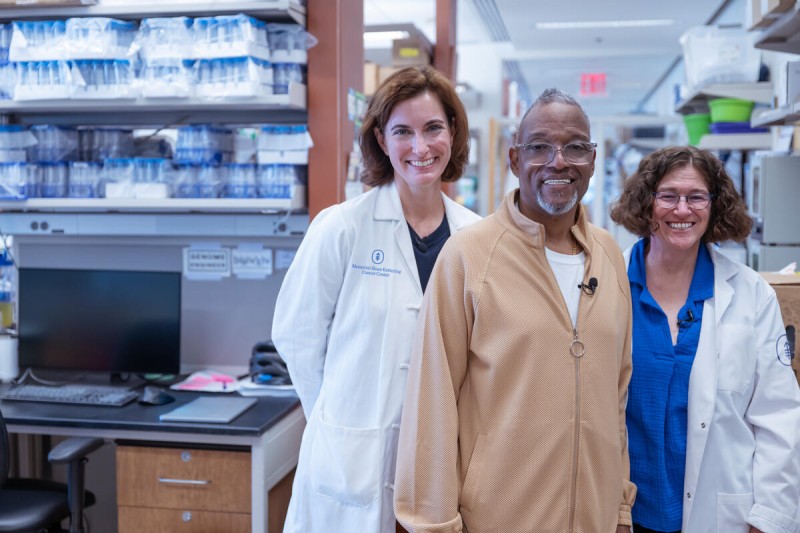
When Carlos Veras started the DFO clinical trial in February 2024, he was in a wheelchair with excruciating back pain caused by stage 4 lung cancer that had spread to his leptomeningeal region. His doctor at another New York City hospital had transferred him to Dr. Boire’s care a few months earlier when the LM was detected.
“I met Dr. Boire, and it was like an angel falling from the sky,” he says. After she carefully explained what the clinical trial would entail, Carlos saw it as his best option.
He started receiving deferoxamine once a week for a month, then transitioned to one dose every two weeks in addition to his other lung cancer treatment. Each session takes 5 to 10 minutes.
The difference two years later is remarkable. Carlos, now 71, gets himself back and forth to MSK like any Bronx resident: He hops on a bus near Yankee Stadium. He takes walks every day, plays with his toddler grandson, goes to the casino every Sunday, and travels once a year.
He knows the treatment is experimental and may not always control the cancer, but he is grateful for the extra time and ability to enjoy his life with his family.
“When you’re in great pain and learn it’s from cancer, you think, ‘This is it,’” Carlos says. “I never would have believed that two years later I would be feeling fine and being able to do all these things.”
Dr. Boire says her team hopes to publish results soon from the first phase of the trial, which is evaluating safety and dosage. More research is needed to determine for certain if the treatment is effective.
“Patients come to MSK from all over the country for the trial because there are vanishingly few clinical trials that study LM,” Dr. Boire says. “This is not a cure by any means, but when we see patients like Carlos wildly outliving expectations, it’s pretty exciting.”
Dr. Boire is the Geoffrey Beene Junior Faculty Chair at MSK.
Dr. Pe’er is the Alan and Sandra Gerry Endowed Chair at MSK.
Key Takeaways:
- Leptomeningeal metastases (LM) occurs where cancer spreads to the cerebrospinal fluid surrounding the brain and spinal cord.
- MSK researchers Adrienne Boire and Dana Pe’er collaborated to discover that cancer cells survive in this space by monopolizing the iron in the leptomeningeal space.
- An MSK clinical trial is testing a treatment that deprives the LM cancer cells of iron.
- While not a cure for LM, the treatment strategy could give patients more time.


