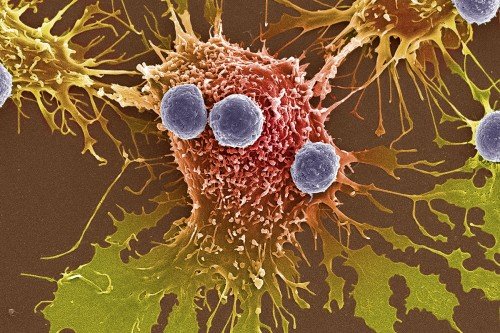
How can oncologists better predict who will benefit from a widely used class of immunotherapy drugs called checkpoint inhibitors?
In the precision medicine era of cancer care, it’s a question that has only increased in relevance. To answer it, a team including Luc Morris, a physician-scientist and research laboratory head, and Nils Weinhold, a computational biology researcher, together with several colleagues at Memorial Sloan Kettering Cancer Center, are looking beyond a known method to predict immunotherapy response.
Tumor mutational burden, or TMB, refers to the number of mutations a tumor has. High TMB means there are a lot of mutations. Low TMB means there are not many mutations. In the past five years, it’s been well established that tumors that have high TMB tend to respond better to checkpoint inhibitor therapy compared with tumors that have low TMB. Because checkpoint inhibitors only work in a fraction of people with cancer, the ability to predict response — like with TMB — is crucial. While TMB can be used to guide treatment decisions for certain patients with cancer — for example, the checkpoint inhibitor pembrolizumab (Keytruda®) is FDA approved for all tumors with high TMB — it remains a “crude predictor” by itself, according to Dr. Morris.
Predicting Immunotherapy Response
“We know that TMB provides some value in predicting immunotherapy response, but we also know that it is not a perfect predictor. It has limited value in isolation,” says Dr. Morris, a senior author on the study, which published November 1, 2021, in Nature Biotechnology.
“Oncologists will consider many factors when deciding on the best treatment for a patient with cancer — TMB is only one,” he says. “For example, a melanoma tumor with low TMB may still have a very good chance of responding, just as a breast tumor with high TMB might have a lower chance of responding. We recognize that we need more predictive tools besides just TMB.”
The study’s co-first authors were Diego Chowell and Steve Yoo, research fellows in the lab of Timothy Chan at MSK, and Cristina Valero, a research fellow in the Morris Lab at MSK. Diego Chowell is currently an assistant professor in the Icahn School of Medicine at Mount Sinai. (Dr. Chan, whose lab first reported the importance of TMB in cancer immunotherapy in 2014, moved to the Cleveland Clinic in 2020.)
The “limited value in isolation” of TMB was one of the reasons why Dr. Morris and fellow investigators wanted to go beyond the biomarker in their latest analysis, he says. Another reason that Dr. Morris undertook this research was to learn more about a blood marker called neutrophil-to-lymphocyte ratio (NLR). Recent MSK research showed that NLR, especially when combined with TMB and other information — such as patient blood markers — could improve the ability to predict tumor immunotherapy response.
“That opened the door for us to say: ‘Why don’t we just gather all of the variables that either have been shown to have predictive value, or that we think might possibly have predictive value, and put them into a machine learning algorithm and see how well we can predict outcomes with a larger pool of information,’” Dr. Morris says.
The team used a model that integrated 16 genomic, molecular, demographic, and clinical features, including TMB and NLR. By taking a machine learning approach, the investigators would be able to determine which combination of variables had the highest predictive power.
“Using this large set of clinical and genomic data from patients treated at MSK, we trained a machine learning model that incorporated a number of different pieces of data,” Dr. Morris explains.
Better than TMB Alone
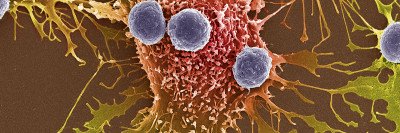
The investigators analyzed the variables in a group of 1,479 patients who were treated with immunotherapy: PD-1/PD-L1 inhibitor immunotherapy, CTLA-4 inhibitor immunotherapy, or a combination of both. Most patients (1,070) did not respond. The group included patients with 16 different types of cancer, of which non-small cell lung cancer and melanoma were the most prevalent. Investigators analyzed patients’ tumors using MSK-IMPACTTM, a powerful tool that provides detailed information about a tumor’s mutations.
“MSK-IMPACT is an incredible resource for us, both as oncologists treating patients and as scientists trying to understand cancer,” says Dr. Morris. “For this study, we had a wealth of genomic data for these patients who were treated at MSK, to integrate with clinical data and blood test data.”
The results reaffirmed TMB’s relevance as a predictor of immunotherapy response; when the variables were studied individually, TMB was associated with the greatest effect of the 16 individual factors.
The next strongest predictors of response to immunotherapy were prior receipt of chemotherapy, albumin levels in the blood, and NLR.
Although each of these four measures could predict immunotherapy response, MSK researchers found that the 16-feature model more accurately predicted response than any one of the individual factors studied alone. What’s more, the 16-feature model was also able to better forecast survival differences among patients who did respond to immune checkpoint blockade and those who did not, further supporting the 16-feature approach over one involving fewer features. Cumulatively, the findings indicate that clinicians can “do better than TMB alone by including other available pieces of information about the patient or the tumor genetics,” Dr. Morris says.
Importantly, the model also takes into account TMB’s varying degrees of predictive value across cancer types, Dr. Morris adds.
“Although the predictive value of TMB varies quite a bit across different cancer types, the [16-feature] model had good predictive ability across all cancer types,” he says. This is important because TMB is less predictive for some malignancies than for others, and for some types of cancer, it has no value at all. For example, the predictive value of elevated TMB is well established in melanoma and non-small cell lung cancer. In breast and prostate cancers, though, TMB has not been found to accurately predict immunotherapy response.
Broad use is part of Dr. Morris and his colleagues’ aim: “This is a very good predictive biomarker based on genetic data from tumor sequencing, but our next research goal will be to try to determine how much value we can glean from a simpler model that maybe could be more widely implemented around the world.”
- Tumor mutational burden, or TMB, is an established way to predict immunotherapy response.
- Although TMB has predictive value for some cancer types, it is not a universal predictor of response.
- Treatment decisions may benefit from including other information along with TMB.
- A machine learning model that can evaluate several predictors of immunotherapy response at once could represent a better approach than those that evaluate singular predictors.
- The machine learning model developed at MSK performed well but requires further study.