MSK surgeons are experts in colorectal surgery for children, teens, and adults. A colorectal (KOH-loh-REK-tul) surgeon is a doctor with special training in surgery on the colon and rectum.
Surgical treatments for colon cancer are similar for children, teens, and adults. MSK Kids colorectal surgeons will adjust the colorectal cancer surgery to the needs and goals of their patient.
What causes colorectal cancer in kids?
Cancers of the colon, rectum, and appendix are rare in children, but they do happen. Most young people who get colorectal cancer have genes that are inherited (passed on to them from their parents). It also can happen without inherited genes. But having these inherited genes means you have a higher risk of getting colorectal cancer.
Some gene changes (mutations or variants) run in a family. By family, we mean people related to you by blood. We also call these family members your blood relatives. They’re not related to you through marriage or adoption.
For example, family members can have an inherited condition called familial adenomatous polyposis (FAP). This disease causes many growths, called polyps, to form in the large intestine.
Another example is Lynch syndrome, also called hereditary nonpolyposis colorectal cancer (HNPCC). There are other inherited conditions that can lead to colon cancer but are less common.
Colorectal surgery for children and adolescents
Surgeons at MSK Kids use minimally invasive methods when possible. Minimally invasive means the surgeon makes small incisions (cuts). This kind of surgery does less harm to the body and has a faster recovery time.
Our surgeons also are experts in surgery methods that keep your child’s healthy colon and rectum safe. Their goal is to cure the cancer while helping young people have the best quality of life.
Minimally invasive surgery with laparoscopy
People who have minimally invasive surgery have less pain and a recover faster than with open surgery.
Surgeons operate through small incisions in the belly using special tools. This is called laparoscopy (LA-puh-ROS-koh-pee). A laparoscope is a long, thin surgical tool with a video camera on the end of it.
Sometimes our surgeons do robotic colorectal surgery using the minimally invasive approach. They use robotic surgery equipment for this operation.
Our colorectal surgeons are also experienced in open surgery when necessary to remove more complex cancers.
Colorectal reconstruction in kids after lower colon removal
For young people who must have their lower colon removed, MSK surgeons may make a special pouch or bag. It’s used to collect bowel movements (poop).
The surgeon loops 2 sections of the small intestine together. Then the wall between them is opened to make a pouch called a J-pouch. The J-pouch makes it possible to go to the bathroom less often after surgery than if you did not have a J-pouch.
Ileorectal anastomosis (rectum sparing surgery for colon cancer)
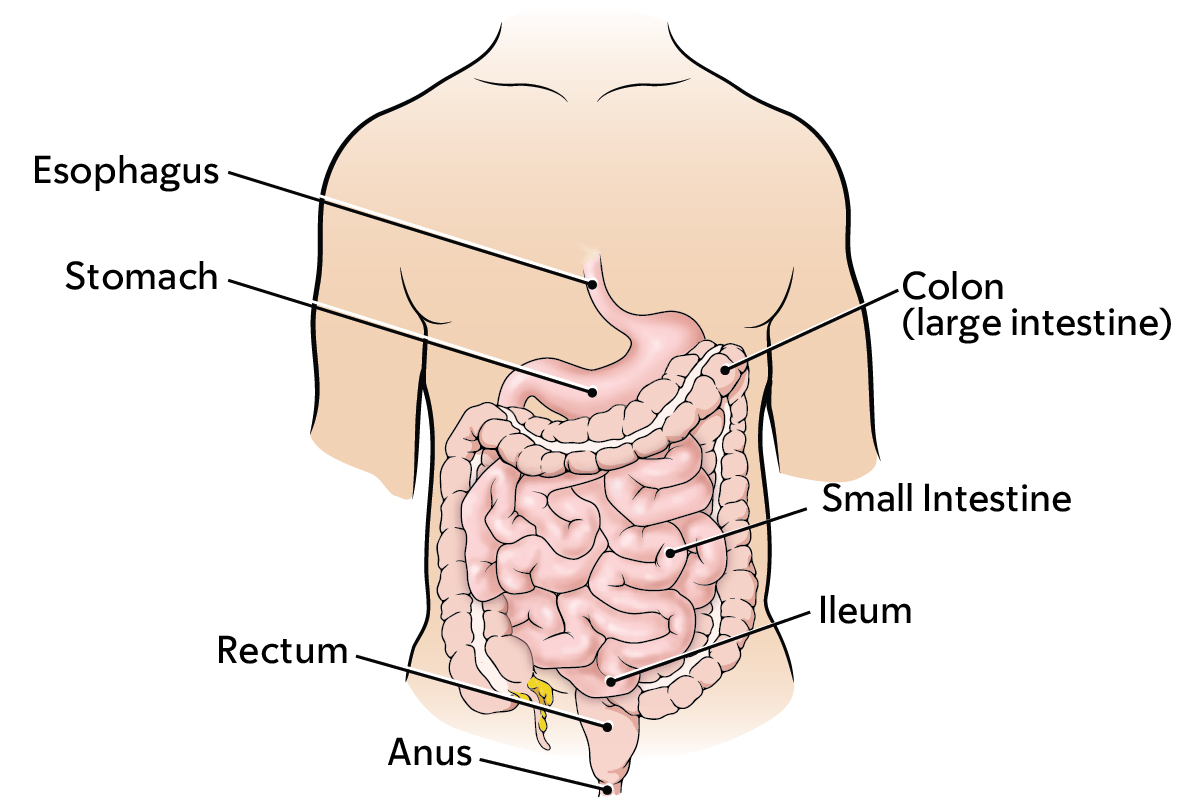
This is a method to save the rectum when the cancer is only in the colon. Surgeons remove the colon. Then the ileum (the end of the small intestine) is attached to the end of the rectum.
Ostomies in young children
Some young people with colorectal cancer need a permanent ostomy. The surgeon will make an ostomy, or stoma, which opens the end of the colon from inside the body to the outside.
An ostomy bag, or pouch, is worn outside the belly to collect bowel movements. Our surgical team understands that temporary ostomies can often be hard for people. That’s very true for young people sensitive about their body image.
We make every effort to avoid ostomies whenever possible. Most of our patients with colorectal cancer do not need permanent ostomies.
Ostomy care for kids
MSK’s wound, ostomy, continence (WOC) nurses are experts at caring for children who have an ostomy. A nurse meets with young people scheduled to have an ostomy to help them get ready for this procedure.
Our WOC nurses provide education and support after surgery, in the hospital and at our outpatient (not at the hospital) locations. We want your child to live the best life possible, even with an ostomy pouch.
Colorectal surgery to lower risk for cancer
This surgery is for children and teens with a very high risk of colorectal cancer. Their higher risk could be hereditary, because of the genes passed on to them from their parents. Or, they could have a higher risk because they have many polyps.
To keep cancer from starting, the surgeon removes part or all of the colon, the rectum, or both. They use minimally invasive surgery and do colorectal reconstruction when possible.
How MSK takes care of your child’s well-being after colorectal cancer surgery
Our colorectal surgeons understand the challenges faced by young people who have colorectal cancer, or are at high risk. At MSK Kids, the concerns and well-being of your child and family are very important to us. Our surgeons will talk with you about care goals.
MSK Kids offers programs and services to take care of your child’s well-being:
- We schedule surgeries to lower your child’s risk for getting cancer according to the school calendar. Surgery can take place over summer vacations or after high school graduation. There’s no need to miss school days.
- We will refer your child for fertility preservation (keeping their ability to make a baby). This includes sperm or egg banking. Some people have trouble having children in the future after being treated for colorectal cancer.
- We connect your child with support for any emotional issues. Children who have had other family members with cancer often need extra support.
- We refer your child and family to the MSK Kids Clinical Genetics Service and Pediatric Cancer Predisposition Screening Program.
Learn more about colon cancer surgery and rectal cancer surgery at MSK.
MSK colon and rectal cancer surgeons

