
Since 1945, the Sloan Kettering Institute has championed a scientific approach to solving the cancer problem.
Engineering Discovery: the Story of SKI
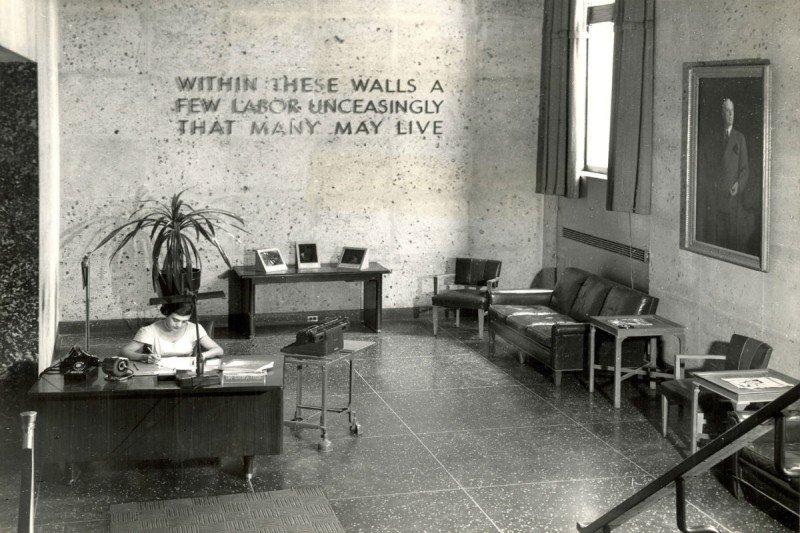
When General Motors executive Alfred Sloan, Jr., and engineer Charles Kettering announced the formation of the Sloan Kettering Institute (SKI) in 1945, they hoped to translate the organizational skills they honed in the automobile industry to the fight against cancer. “I am inclined to feel we can apply some of our time-tried techniques to this age-old problem,” Mr. Kettering said.
In essence, that meant providing scientists with the time, financial support, and technological resources to do what they do best: conduct research.
As an institute devoted to research, SKI’s mission has always been to supply the raw material of discovery out of which new approaches to cancer treatment, diagnosis, and prevention emerge. The first chemotherapy drugs, the first immune-based treatments for cancer, and a variety of targeted therapies all had their origins at SKI.
- The first chemotherapy drugs, including the nitrogen mustards and 6-MP
- Neupogen (filgrastim), a drug that helps blood cell counts recover after chemotherapy
- Vorinostat (Zolinza), the first HDAC inhibitor
- Ipilimumab (Yervoy), the first immune checkpoint inhibitor
- Chimeric antigen receptor (CAR) T cells, sometimes called “living drugs”
1945–1959: Birth of Chemotherapy
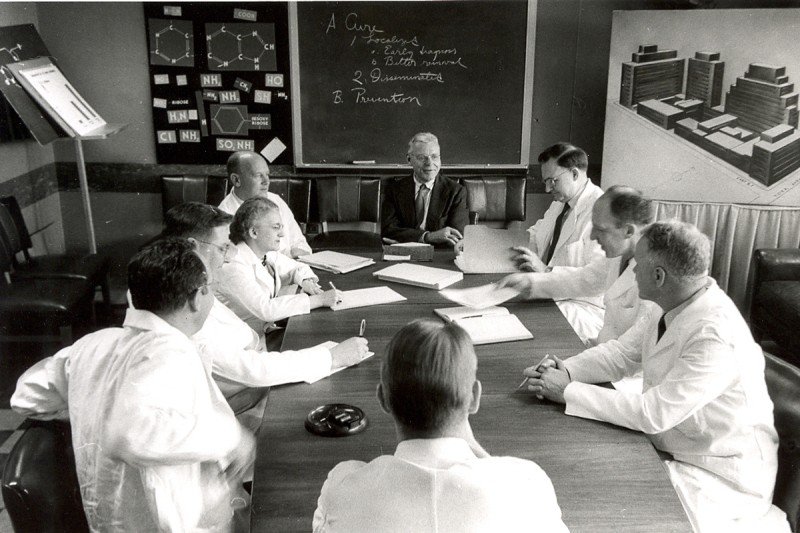
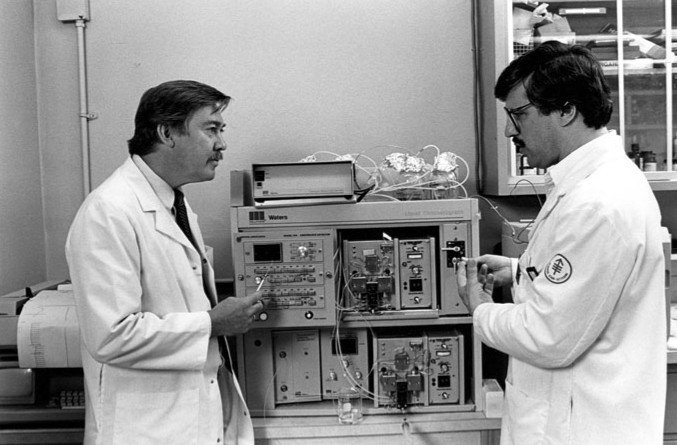
Nothing better illustrates the early aspirations of the institute than the search for effective chemotherapeutic drugs. This massive program involved screening more than 50,000 natural and human-made chemicals for their effectiveness as anticancer drugs. It would lead to the development of some of the first approved chemotherapy drugs, and also served as a model for a similar program at the National Cancer Institute.
SKI’s first director, a pathologist named Cornelius Rhoads, had served as chief medical officer of the Army’s Chemical Warfare Service during World War II. From this post, he learned about the effects of chemical weapons, such as mustard gas, on human physiology. Research in this area eventually led to the development of the class of chemotherapy drugs called the nitrogen mustards. Dr. Rhoads’s ties to the military and charges of unethical human experimentation would later sully his reputation as a pioneer of chemotherapy.*
SKI also supported the work of chemists Gertrude Elion and George Hitchens at Burroughs Wellcome, which produced the chemotherapy drug 6-mercaptopurine (6-MP). MSK oncologists Joseph Burchenal and David Karnofksy led the testing of this new compound in people with leukemia. Based on this work, the US Food and Drug Administration approved 6-MP in 1953.

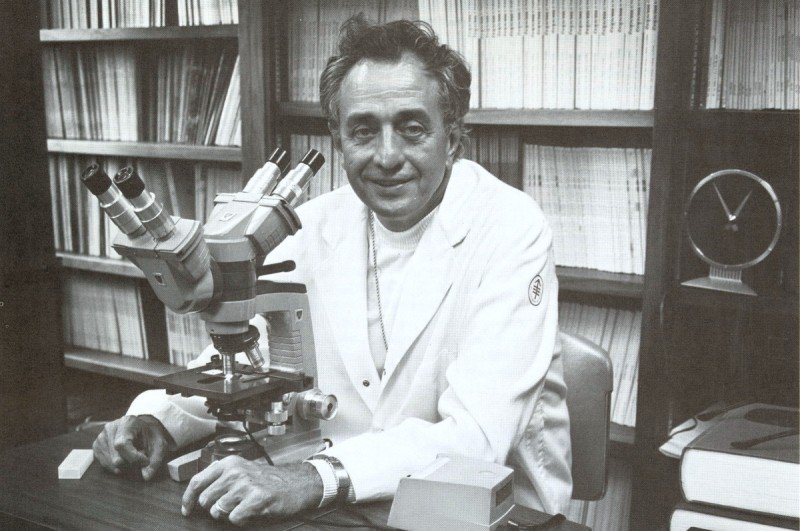
In 1958, a young medical doctor joined the experimental chemotherapy division at SKI. His interests were slightly different from those of his fellow chemotherapists. What captured Lloyd Old’s imagination was the idea that the immune system could fight cancer.
In 1959, Dr. Old, along with his colleagues Baruj Benacerraf and Donald Clarke, showed that mice injected with a germ called BCG could fight off transplanted tumors and resist new tumors forming. This was a seminal moment in immunotherapy. Dr. Old is considered the father of modern tumor immunology.
1960–1979: Viruses, Cancer, and Immunity
Dr. Rhoads, SKI’s first director, died suddenly in 1959. Replacing him, in 1960, was Frank Horsfall, a pioneering virologist who had studied the influenza virus at the Rockefeller Institute, next door to Memorial Hospital. As director, Dr. Horsfall encouraged the study of virology and immunology at SKI.
He supported the work of several scientists who were studying the relationship between viruses and cancer, for example, including Alice Moore, Charlotte Friend, and Chester Southam. These researchers identified cancer-causing viruses and, conversely, also showed that infection with some viruses causes cancers to regress. These developments were a forerunner of today’s oncolytic virus therapies.
Having established in 1959 that the immune system could fight cancer, SKI immunologist Lloyd Old next went in search of distinguishing cancer markers, or antigens, and the cell types involved in immune recognition. In the early 1960s, with SKI geneticist Edward (Ted) Boyse, he identified cancer antigens associated with chemically induced and virally caused cancers. Later, the same team discovered that immune cell types could be distinguished by specific cell-surface markers, which led to the identification of CD8+ “killer” T cells and CD4+ “helper” T cells.
The immunological focus of the institute continued under its third director, Robert Good, who served from 1973 to 1980. Dr. Good was a pioneer of bone marrow transplantation, having achieved the first successful cure of a boy with an immune disorder called SCID.
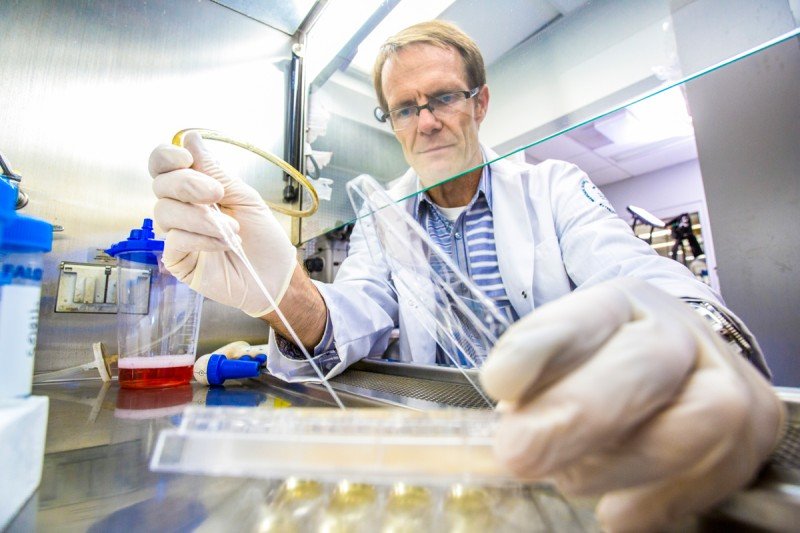
Hematologist and cell biologist Malcolm Moore came to SKI in 1974. Work that he conducted on factors that stimulate blood growth would lead to the development of the drug Neupogen (filgrastim). This widely used medicine helps blood cell counts recover after chemotherapy, reducing the risk of infection and hospitalization. It is one of the most important cancer drugs ever developed.
1980–1999: Getting Molecular
By the end of the 1970s, the field of molecular biology was exploding, offering new ways to understand and manipulate the DNA within cells. SKI would need to make some changes to take advantage of the new perspective.
The person who did the most to bolster SKI’s expertise in molecular biology was Paul Marks, a physician-scientist who served as MSK’s president from 1980 to 1999. It was Dr. Marks’s belief that this area held great promise for understanding and treating cancer.
Dr. Marks’s views on cancer research were shaped in part by his own introduction to molecular biology, through time he spent in the Pasteur Institute lab of the Nobel Laureate Jacques Monod in the 1960s. He wanted to bring that perspective to MSK.
“Most of the answers to cancer lie down on the level of the genes, in our understanding of how cells differentiate and divide,” Dr. Marks once said. He appointed physician-scientist Richard Rifkind director of SKI in 1983 to help him grow the institute. Dr. Rifkind was a colleague from Columbia, where both he and Dr. Marks were faculty before coming to MSK.
Among the talented scientists that they recruited to SKI in the 1980s were Jerard Hurwitz and Ora Rosen, who founded the Molecular Biology Program. Dr. Hurwitz had co-discovered the enzyme RNA polymerase in 1960. Dr. Rosen was a world expert in the biology of hormones. In 1985, Dr. Rosen was part of a team, including members of the newly founded company Genentech, that cloned the gene for the insulin receptor.
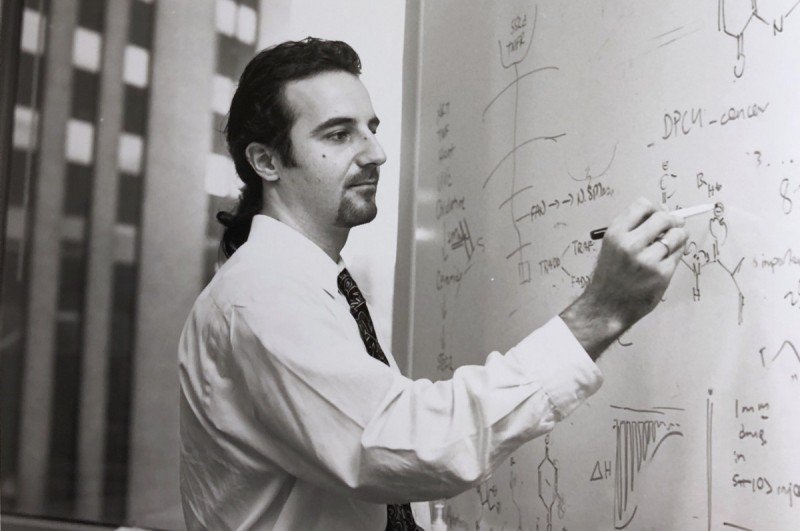
Cancer biologist Joan Massagué arrived at SKI in 1989 as the new chair of the Cell Biology Program. After joining SKI, Dr. Massagué elucidated the transforming growth factor beta (TGF-beta) signaling pathway. This pathway controls several aspects of cell behavior and is often derailed in cancer.

The 1990s witnessed substantial growth in biochemistry and biophysics. James Rothman arrived in 1991, becoming founding chair of the Cellular Biochemistry and Biophysics Program. A giant in the field, Dr. Rothman would go on to receive a Nobel Prize, in 2013, for his work on protein trafficking done at SKI.
Structural biology also gained momentum at this time. One of the first recruits, Dinshaw Patel, did some of the earliest work linking chemical carcinogenesis to DNA binding. Another, Nikola Pavletich, deciphered the detailed atom-by-atom structure of several key proteins involved in sensing DNA damage and repairing it, including p53, RecA, BRCA2, and others.
2000–2009: Expanding Cancer Research
Dr. Marks ended his 19-year tenure as MSK president in 1999. The person who succeeded him, Harold Varmus, had received a Nobel Prize in 1989 for his co-discovery, with J. Michael Bishop, of the cellular origin of viral oncogenes. A preeminent scientist and an accomplished administrator who had previously led the National Institutes of Health, Dr. Varmus was a natural choice to grow the stature and quality of research at SKI.
Dr. Varmus redoubled the institute’s commitment to the pursuit of scientific research, growing the number of programs and faculty in SKI. In 2002, he appointed Thomas Kelly to be SKI director. Dr. Kelly had overseen the creation of a world-class molecular biology program at Johns Hopkins University, and Dr. Varmus recognized him as a keen spotter of talent as well as a capable administrator.
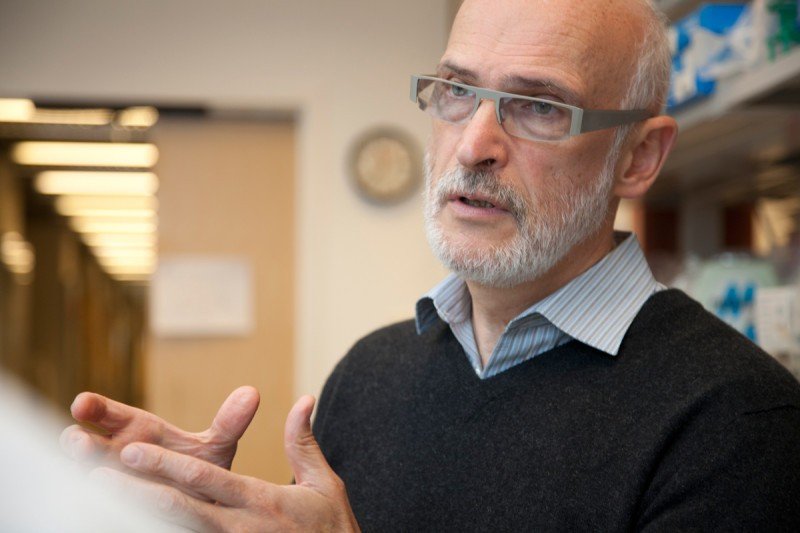
Among the individuals Dr. Kelly recruited was immunologist James Allison, who arrived at SKI in 2004 and became chair of Immunology. In his previous position, at the University of California, Berkeley, Dr. Allison had discovered that a molecule called CTLA-4 acts as a brake or checkpoint on immune cells, restraining them from attacking. Releasing this brake with an antibody, he found, could cure cancer in mice. This work led eventually to the development of the first immune checkpoint inhibitor, ipilimumab. Dr. Allison’s decision to come to SKI was influenced by the opportunity to work closely with clinical researchers to shepherd his laboratory findings through the drug development pipeline all the way to patients.
“It’s a great example of how basic knowledge — in this case about how immune cells function — can lead to major new cancer breakthroughs,” Dr. Kelly says.



In addition to recruiting new talent, Dr. Kelly also reorganized the institute’s structure, first by dividing up the Molecular Biology Program.
“Molecular Biology was a funny program at that time,” says developmental biologist Kathryn Anderson, who arrived at SKI in 1996. “It was sort of half nucleic acids biochemistry and half development biology. It was an unusual marriage of these two very different interest groups.”
In 2002, Dr. Kelly split molecular biology and development into separate programs and assigned new leadership. Dr. Anderson became chair of Developmental Biology, while Ken Marians, an expert in DNA replication, remained chair of Molecular Biology.
Dr. Kelly also split Structural Biology off from Cell Biology, and created a new program in Cancer Biology and Genetics. Dr. Massagué, who had been chair of Cell Biology, was named the inaugural chair of this innovative new program that sought to bridge experimental and clinical aspects of cancer research. Alan Hall, who discovered the function of Rho GTPases in controlling the actin cytoskeleton, was brought in to lead Cell Biology in 2006.
Dr. Kelly was also influential in starting the Gerstner Sloan Kettering Graduate School of Biomedical Sciences (GSK). Although SKI had been involved in education since 1950, when it began allowing students from Cornell University Graduate School of Medical Sciences to conduct their research in SKI labs under the guidance of SKI faculty, it did not have a school of its own. GSK would take advantage of what was unique about the educational opportunity of SKI, namely the close collaboration between scientists and clinicians. GSK admitted its first class of students in 2006.
2010–today: Science to and from the Clinic
When Craig Thompson became president and CEO of MSK in 2010, he sought to bring about even more fruitful collaborations between scientists and clinicians across the institution. “I want us to realize the full clinical potential of all the extraordinary research that goes on here,” Dr. Thompson said.
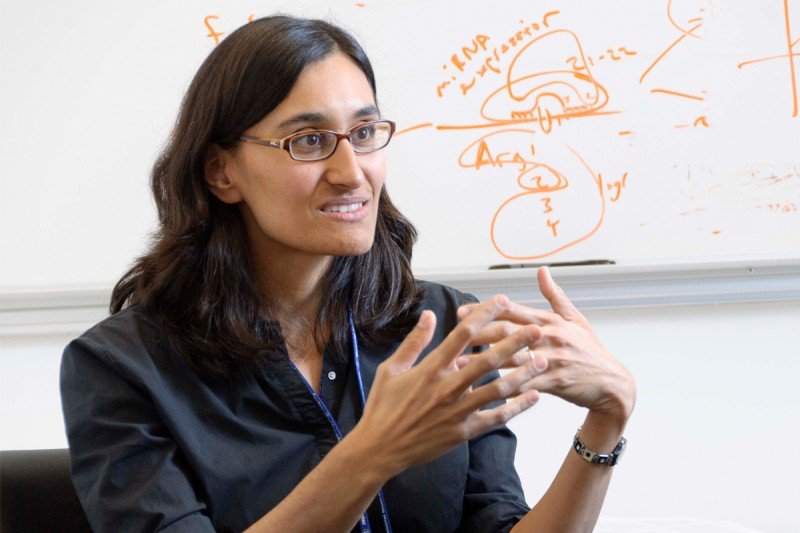
To help execute that plan, he appointed Dr. Massagué as director of SKI. Having chaired both the Cell Biology Program and the Cancer Biology and Genetics Program, Dr. Massagué had a proven track record of leadership. He also shared Dr. Thompson’s belief in the power of collaboration between scientists and clinical researchers. Together, they worked to strengthen the research capabilities and collaborative opportunities across MSK.
Dr. Massagué established new programs in Chemical Biology and Computational & Systems Biology, and new collaborative research centers — the Metastasis and Tumor Ecosystems Center and the Center for Epigenetics Research.
He also initiated projects that seek to take maximal advantage of discoveries emerging from the clinic to bolster research into the principles of biology. The Functional Genomics Initiative, for example, brings findings about drug responsiveness — who responds and who doesn’t — back to researchers in SKI. They can then work out the molecular basis for these clinical results.
“SKI is the preeminent entity for basic, preclinical, and postclinical research in cancer science,” Dr. Massagué says.
Once considered too complicated to study, human biology has become a main focus of researchers in the institute. The ability to sequence human DNA and to analyze human tumor tissue with advanced microscopy techniques have allowed researchers to draw direct links between findings in mice and other model organisms to human cancers. Increasingly, SKI researchers are tapping what Dr. Massagué calls “the awesome power of the human as a model organism.”

An emerging focus of the institute is the study of epigenetics — chemical modifications to DNA and chromatin that affect gene regulation. Investigators from several different SKI programs work in this area, which has ramped up in recent years.
SKI is also expanding computational biology and its application of single-cell analysis to the study of cellular and genetic complexity of developing tissues and tumors.
The role of the immune system — both innate and adaptive — in restraining and shaping cancer development continues to be a strong focus of research at SKI. Researchers explore the biology of inflammation, natural killer cells, and the role of regulatory T cells in health and disease, among other topics.
The biology of metastasis, the role of the microbiome in health and disease, and the biology and applications of stem cells are all active areas of research. Scientists are even returning to the study of cancer metabolism, thanks to insights and discoveries made by Dr. Thompson, also a member of the Cancer Biology and Genetics Program.
Though much has changed at SKI since 1945, the underlying philosophy of the institute remains the same. “Although many investigators pursue research with an eye toward having an impact in the clinic,” Dr. Massagué says, “investigators must be free to pursue whatever their instinct tells them will provide the most penetrating insights into the unknown.”
Read more about recent discoveries and advances emerging from the Sloan Kettering Institute.