
Even a successful treatment can be improved, to give patients more options, including fewer side effects.
That is the benefit of an important clinical trial (research study) involving rectal cancer treatment without radiation that was announced in early June at the American Society of Clinical Oncology (ASCO) annual meeting, the country’s largest cancer conference. The study also published in The New England Journal of Medicine.
This research is led by gastrointestinal oncologist Deb Schrag, MD, MPH, Chair of the Department of Medicine at Memorial Sloan Kettering Cancer Center (MSK).
Radiation-Free Rectal Cancer Treatment Clinical Trial Results
The trial involved more than 1,100 people with locally advanced rectal cancer, meaning it had not spread to other organs. After five years, the research found that people who received a type of chemotherapy regimen called FOLFOX alone before surgery did just as well as those who underwent both chemotherapy and radiation before surgery. Skipping radiation could mean improvements in patients’ quality of life, including the preservation of fertility, sexual function, and more.
Dr. Schrag says: “There are around 47,000 people diagnosed with rectal cancer every year. We believe around 20,000 of them — who have stage 2 or 3 cancer — could benefit from this approach that can spare them from having to get radiation in addition to chemotherapy and surgery.”
Side Effects From Standard Treatment for Rectal Cancer
Typically, a person diagnosed with rectal cancer will receive radiation to the pelvic area given together with 5FU chemotherapy, either intravenously (in the vein) or orally (in the mouth). This strategy is known as chemoradiation and is sometimes referred to as 5FUCRT. The next steps are surgery to remove the tumor and, usually, more chemotherapy to keep the cancer from coming back in a distant organ.
“We’ve used chemoradiation since 1990 because it’s been remarkably effective at reducing the rate of local recurrences in the pelvis,” Dr. Schrag says. “This is critical because pelvic recurrence of rectal cancer is difficult to treat and causes much suffering. Since 2004, we have given the chemoradiation before surgery.”
But Dr. Schrag and colleagues wondered if they could get the same outcomes without subjecting patients to the side effects radiation often causes in such a complex region of human anatomy.
The rectum is the last six inches of the digestive system. It sits inside the pelvis, which is a crowded neighborhood of bone and tightly packed organs. Radiating this area can damage reproductive organs, cause infertility, and lead to early menopause in women, among other side effects.
“My colleagues and I began seeing more young women with rectal cancer who were devastated — not just because they had cancer but because the standard treatment we had to offer them would mean that they would not be able to carry a pregnancy to term,” Dr. Schrag says. “That was one of the big reasons we looked for a way to help patients and to see if we could achieve favorable outcomes without the uniform application of radiation.”
Dr. Schrag believes these issues are particularly urgent today because a growing number of people are diagnosed with rectal cancer at young ages — when fertility concerns are especially important. MSK is a leader in trying to find out why rectal cancer is rising among younger adults and established the first center in the world devoted to their specific needs: the Center for Young Onset Colorectal and Gastrointestinal Cancer.
People facing rectal cancer, Dr. Schrag says, are often concerned about other long-term consequences of radiation, which can impair (damage or weaken) bowel and sexual function.
There are also concerns about radiation and bone marrow, which makes blood. “Most of your bone marrow is made in the pelvic bones. When you radiate those bones, the bone marrow resilience can be impaired,” she says. That’s important, she adds, because “if the cancer comes back, it’s more difficult to give you chemotherapy if your bone marrow reserve is impaired.”
The PROSPECT Clinical Trial for Rectal Cancer: Replacing 5FUCRT With FOLFOX
Dr. Schrag and colleagues decided to turn the standard-of-care treatment on its head to address concerns about side effects.
The seed for the clinical trial idea started to sprout during MSK Colorectal Service meetings, where specialists from across disciplines discuss complex cases of rectal cancer. “MSK colorectal surgeon Martin Weiser, MD; gastrointestinal oncologist Leonard Saltz, MD; radiologist Marc Gollub, MD, and I launched a pilot trial to test the effectiveness of the idea,” Dr. Schrag says. “It was a small study of just 30 patients, but it enabled us to persuade our colleagues nationally to test the approach in a randomized trial.”
The chemotherapy regimen that is usually given after surgery for rectal cancer is called FOLFOX, which includes the drugs 5-fluorouracil (5FU), oxaliplatin, and leucovorin. Preliminary research showed that giving FOLFOX before surgery could also have good results, which Dr. Schrag confirmed in a pilot trial.
She hypothesized that giving FOLFOX alone before surgery — without radiation — could provide patients with the same good outcomes as the standard of care.
The trial, named PROSPECT, had two arms. One arm used FOLFOX chemotherapy before surgery and only used radiation if the response to FOLFOX alone was not sufficient (this happened for less than 10% of patients). The other arm used chemoradiation before surgery.
More than 1,100 patients were evenly split between the two arms, with patients participating at medical centers around the U.S. and Canada.
After five years, the results were clear: The patients who received only FOLFOX before surgery did just as well as the patients who received chemoradiation. Major endpoints, including disease-free survival, overall survival, and the rate of cancer recurrence, were nearly identical between the two methods.
The new method showed other benefits. For instance, the number of patients who needed a temporary ostomy was lower when radiation was not used. An ostomy is a surgically created hole in the abdomen (belly) that allows waste to be transported to a pouch outside the body. Ostomies are usually temporary for patients with rectal cancer that has not spread, but finding that fewer patients needed them at all after treatment with the new method was a definite improvement in quality of life.
Radiation for Rectal Cancer May Still Be Necessary for Some
Dr. Schrag is careful to point out that while the new method offers patients and doctors another option, in some cases radiation before surgery is still preferred. “In about 10% of cases, the person did not respond well enough to the FOLFOX regimen, and we administered chemoradiation,” she says.
Also, FOLFOX chemotherapy alone before surgery requires longer rounds of treatment, which can mean more side effects initially, including neuropathy of the hands — numbness or sharp pain.
Chemotherapy and surgery do have side effects, Dr. Schrag says, but this study found that patients with rectal cancer have options that don’t involve radiation. “Particularly for people concerned about radiation affecting their fertility,” she adds, “the new FOLFOX regimen presents an alternative.”
A Patient’s Successful Treatment Without Radiation Therapy
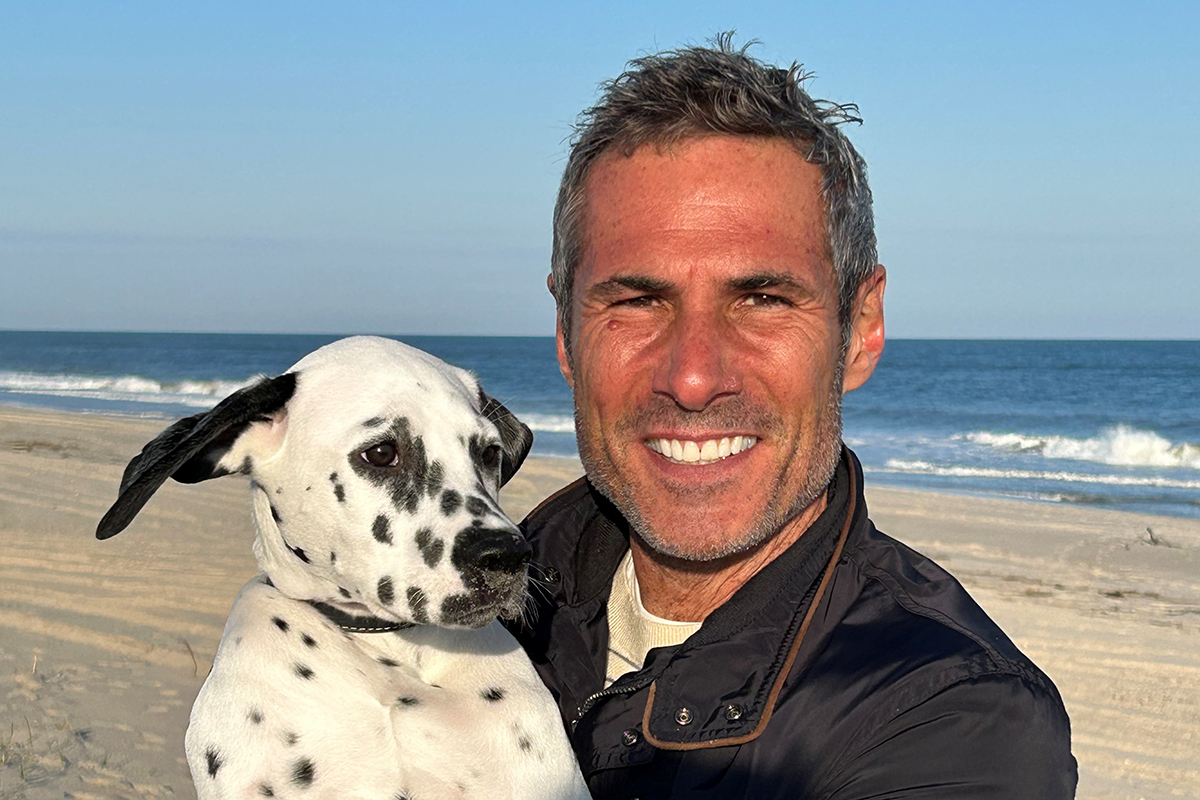
Having treatment options was important to Marc Scarduffa. He felt healthy and symptom-free when he underwent his first colonoscopy at age 50. (At the time, 50 was the recommended age to begin colorectal screening. It has since been lowered to 45 for people at average risk.)
Marc was stunned when the test revealed a stage 3 rectal cancer tumor. Marc had spent much of his career leading government relations for a major pharmaceutical company and was well-versed in medical issues. “I started at another hospital, but I insisted on MSK because it’s the gold standard.”
At MSK, Marc was cared for by Drs. Saltz and Weiser. Marc says their compassion and concern for his quality of life immediately reassured him. “I had been planning a big 50th birthday party in Italy, and Dr. Saltz said: ‘Go and enjoy it. We’ll start when you come back.’ That made such a difference, to spend time with family and friends.”
On Marc’s return, Drs. Saltz and Weiser told him about the clinical trial of treatment without radiation. “I had heard from several people about side effects they endured with radiation,” Marc says. “I was very happy to have an opportunity to not get radiation and instead just have FOLFOX and surgery.”
For Marc, the chemotherapy had only minor side effects. “Most people didn’t know I had cancer,” he says. “I was very enthusiastic about not having to lose my hair to radiation, and I continued to travel often for work.” After recovering from surgery, Marc returned to health and says the clinical trial was definitely the right option for his care.
“I’m such a big fan of MSK, and I’ve told several other people facing cancer to go there. I felt a real bond with my doctors.”
Radiation-Free Rectal Cancer Treatment Can Help Patients in Rural Areas
The new method may also benefit patients who face challenges of geography in addition to their cancer diagnosis.
“If you live in Idaho or Montana or many other rural parts of America, you may be many hours away from anywhere you can receive radiation treatment,” Dr. Schrag says. Chemoradiation requires 28 daily visits over five and a half weeks. In comparison, FOLFOX requires about six visits over 12 weeks. “For some people, the schedule and convenience are important.”
That benefit is magnified globally, because radiation treatment facilities are scarce in some countries, Dr. Schrag says. “In some parts of the world, access to radiation is very limited. Chemotherapy may be a more accessible alternative.”
Collaboration Is Key to Breakthrough Discoveries
This research was funded by the National Cancer Institute, a federal effort that is part of the National Institutes of Health. “These are your taxpayer dollars at work,” Dr. Schrag says. “This is the kind of work that only the government will fund because there is no commercial sponsor.”
Making use of those resources to accomplish the PROSPECT trial was possible “because of strong leadership from different disciplines,” she adds. “Management of rectal cancer is a team sport.”
The PROSPECT team included Dr. Weiser (Colorectal Surgery); Ellen Hollywood, RNP (Nursing); Dr. Saltz (Medical Oncology); Dr. Karyn Goodman (Radiation Oncology, now at Mount Sinai); Dr. Gollub (Radiology); and Jinru Shia, MD (Pathology).
Dr. Schrag also looks forward to the “next generation of MSK investigators, including gastrointestinal oncologist Andrea Cercek, MD; gastrointestinal oncologist Rona Yeager, MD; gastrointestinal oncologist Michael Foote, MD; surgical oncologist Josh Smith, MD, PhD, and others.” She believes they will “lead the next generation of trials that will improve outcomes still further for patients with rectal cancer.”
Dr. Schrag says her deepest thanks go to the courageous patients who participated in the trial. “It’s not easy to say to a patient, ‘Let’s try treating you by omitting a treatment that has been used for over two decades,’ ” she says. “My hope is that this treatment approach will give people with rectal cancer and their doctors a new option. At MSK, our mission is to keep pushing the boundaries to make meaningful differences for our patients.”
Disclosures: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers U10CA180821, U10CA180882, UG1CA189823 (to the Alliance for Clinical Trials in Oncology), UG1CA232760, UG1CA233180, UG1CA233290, UG1CA233329, UG1CA233373, P30 CA008748, P30CA006516, U10CA180863, CCS#707213 (CCTG), U10CA180820 (ECOG-ACRIN), U10CA180868 (NRG), and U10CA180888 (SWOG), and the Swiss Group for Clinical Cancer Research (SAKK).
