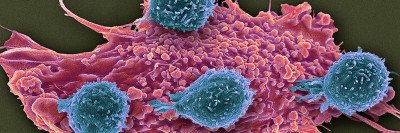
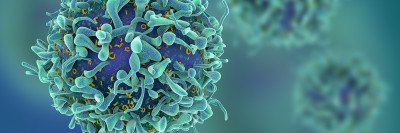
Checkpoint inhibitors work by releasing a natural brake on your immune system so that immune cells called T cells recognize and attack tumors.
This therapy is sometimes called immune checkpoint blockade because the molecule that acts as a brake on immune cells — the checkpoint — is blocked by the drug.
Our researchers have played a leading role in developing checkpoint inhibitors and demonstrating their safety and effectiveness in cancer patients.
MSK has helped lead several clinical trials showing that checkpoint inhibitors can be effective against melanoma and lung cancer, and these drugs are being tested at MSK against sarcoma, lymphoma, and several other cancers.
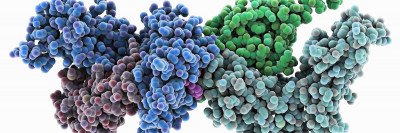
One drug called ipilimumab (Yervoy®) blocks a checkpoint protein called CTLA-4. Two additional drugs, pembrolizumab (Keytruda®) and nivolumab (Opdivo®), target another checkpoint protein called PD-1. A third drug, atezolizumab (Tecentriq®), targets one called PD-L1.These drugs all became available within the last few years. The US Food and Drug Administration (FDA) approved ipilimumab in 2011 and pembrolizumab and nivolumab in 2014, all for the treatment of melanoma. In 2015, the FDA also approved nivolumab and pembrolizumab for non-small cell lung cancer, and nivolumab for renal cell carcinoma.
Several additional checkpoint drugs are being studied and investigated in clinical trials at MSK.
Patients Receiving Immune Checkpoint Blockade Therapy
Immune checkpoint inhibitors are given through a vein in your arm (intravenously). The treatment period usually lasts 30 to 60 minutes; the number of sessions may vary depending on your cancer and the drug you’re being given.
If you’re receiving ipilimumab (Yervoy®), you’ll probably receive treatment at our Rockefeller Outpatient Pavilion once every three weeks for a total of four treatments. If you’re receiving pembrolizumab (Keytruda®) or nivolumab (Opdivo®), you’ll likely come for treatment every other week for a longer period — sometimes up to a year or more. Before each session, you’ll first meet with your medical oncologist or nurse practitioner before proceeding to the infusion suite to receive the drug.
Immune checkpoint inhibitors are generally less toxic and easier to take than most chemotherapy drugs. Unlike some chemotherapies, these immunotherapy drugs do not require you to have a port — a round metal or plastic disk that is used as the entry site for the IV medications — surgically implanted in your body. Immune checkpoint drugs also don’t involve pretreatment preparation, such as hydration, that chemotherapy drugs sometimes require.
Our doctors and nurses are experts in caring for the complex needs of patients undergoing outpatient immunotherapy treatment. If you experience any side effects from immunotherapy drugs, our medical care specialists are highly trained to help you manage them.