This information explains the procedure to place your CVC, including how to get ready and what to expect. It also explains how to care for your CVC. In this resource, the words “you” and “your” refer to you or your child.
About CVCs
A CVC is a catheter (long, flexible tube) that’s put into a vein in your chest. There are many types of CVCs. Your doctor will decide which type is best for you.
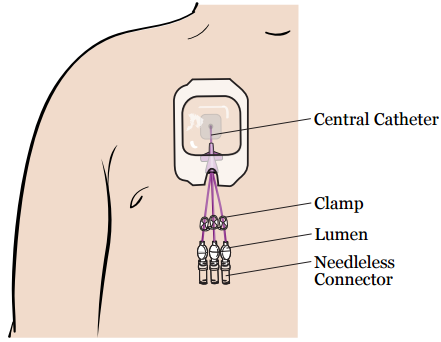
All CVCs have 1 central catheter that’s put into a large vein near your heart. Outside your body, the central catheter divides into 1, 2, or 3 smaller tubes called lumens. Each lumen has a clamp, a needleless connector, and a disinfection cap on the end (see Figure 1). A needleless connector is sometimes called a clave.
Having a CVC will help you need fewer needle sticks. Your care team can use your CVC to:
- Take blood samples.
- Give you fluids.
- Give you chemotherapy and other medications.
- Give you blood transfusions.
- Give you intravenous (IV) nutrition.
Your CVC can stay in your body for as long as a few years. It will stay in place for your whole treatment. Your doctor will remove your CVC when you don’t need it anymore.
Having a CVC should not keep you from doing your normal activities. This includes going to school or work, showering, and doing light exercise. Read the section “Caring for Your CVC” to learn more.
You’ll have a procedure to place your CVC. Your nurse will tell you how to get ready for your procedure. They’ll also teach you how to care for your CVC after your procedure.
You’ll learn to:
- Change your needleless connectors.
- Change your disinfection caps, such as SwabCaps®.
- Flush your CVC.
Your healthcare provider may teach you how to change the dressing. You can have a caregiver, family member, or friend learn with you. After you go home, use this resource to help you remember the steps to care for your CVC.
What to do before your procedure
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Take only the medicine your surgery team told you to take the morning of your procedure. If you don’t, we may need to cancel your procedure. Take them with a few sips of water.
Anticoagulants (blood thinners)
If you take a blood thinner, ask the doctor who’s doing your procedure what to do. Blood thinners are medicines that affects the way your blood clots.
| Examples of Blood Thinners | |
|---|---|
|
|
Medicine for diabetes
If you take insulin or other medicine for diabetes, you may need to change the dose. Talk with the healthcare provider who prescribes your diabetes medicine about what to do the morning of your procedure.
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
If you have pain or discomfort, take acetaminophen (Tylenol®). Do not take more acetaminophen than directed on the label or as instructed by your healthcare provider.
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment
Tell us if you’re sick
If you get sick before your procedure, call the healthcare provider who scheduled your procedure. This includes a fever, cold, sore throat, or the flu.
What to do the day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
This will be one of the following places:
-
Pediatric Ambulatory Care Center (PACC)
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to the 9th floor. -
Presurgical Center (PSC) on the 6th floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to the 6th floor.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
Shower with a 4% CHG solution antiseptic skin cleanser, such as Hibiclens
Shower with a 4% CHG solution antiseptic skin cleanser before you go to bed the night before your procedure.
Instructions for using 4% CHG solution
- Wash your hair with your usual shampoo and conditioner. Rinse your head well.
- Wash your face and genital (groin) area with your usual soap. Rinse your body well with warm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Do not put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne after your shower.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
What to do the day of your procedure
Instructions for drinking before your procedure
You can keep drinking formula, breast milk, and clear liquids after midnight. Follow the instructions in the table below. It’s OK to brush your teeth and take your medications with a small sip of water.
| Type of liquid | Amount to drink | When to stop drinking |
|---|---|---|
| Formula | Any amount | Stop drinking formula 6 hours before your scheduled arrival time. |
| Breast milk | Any amount | Stop drinking breast milk 4 hours before your scheduled arrival time. |
| Clear liquids such as water, fruit juice without pulp, carbonated (fizzy) drinks, tea without milk, and coffee without milk |
| Stop drinking clear liquids 2 hours before your scheduled arrival time. |
Do not drink anything starting 2 hours before your scheduled arrival time. This includes formula, breast milk, water, and other clear liquids.
Take your medicines as instructed
A member of your care team will tell you which medicines to take the morning of your procedure. Take only those medicines with a sip of water. Depending on what you usually take, this may be all, some, or none of your usual morning medicines.
Things to remember
- Wear clean, comfortable clothing.
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during a procedure can damage your eyes.
- Do not wear any metal objects. Remove all jewelry, including body piercings. The tools used during your procedure can cause burns if they touch metal.
- Leave valuable items at home if you don’t need them. This includes extra credit cards, extra cash, and jewelry.
- If you’re menstruating (have your monthly period), use a sanitary pad, not a tampon. You’ll get disposable underwear, as well as a pad if needed.
What to bring
- A list of the medicine you take at home. This includes over-the-counter and prescription medicine, patches, and creams.
- Medicine for breathing problems, such as inhalers, if you take any.
- Medicine for chest pain, if you take any.
- A case for your glasses or contacts.
- Your Health Care Proxy form and other advance directives, if you’ve completed them.
- Your breathing device for sleep apnea, such as your CPAP or BiPAP, if you have one.
- This resource. You’ll use it to learn how to care for your CVC after your procedure.
Once you’re in the hospital
When you get to the hospital, take the B elevator.
- If you’re going to the PACC, take the elevator to the 9th floor.
- If you’re going to the PSC, take the elevator to the 6th floor.
Many staff members will ask you to say and spell your name and date of birth. This is for your safety. People with the same or a similar name may be having a procedure on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown, robe, and non-skid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches and creams.
Your nurse may place an intravenous (IV) line into one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Get ready for your procedure
One or 2 visitors can keep you company as you wait for your procedure to start. When it’s time for your procedure, a staff member will bring your visitor(s) to the waiting area.
Before you go into the procedure room, you may need to remove certain items, if you have them:
- Hearing aids
- Prosthetic devices
- Wig
- Religious items
You’ll either walk into the operating room or a staff member will bring you on a stretcher. A member of the procedure room team will help you onto the procedure bed. Once you’re comfortable, your anesthesiologist will give you anesthesia through your IV line and you’ll fall asleep.
During your procedure
First, your doctor will give you an injection (shot) of local anesthesia near your collarbone. Local anesthesia is a medicine that makes an area of your body numb. This will help keep you from having pain after your procedure.
Next, your doctor will make 2 small incisions (surgical cuts) called the insertion site and exit site.
- The insertion site is where your CVC will enter your vein. This incision will be just below your collarbone.
- The exit site is where your CVC will leave your body. This incision will be a few inches below the insertion site.
Then, your doctor will place one end of your CVC through the insertion site and into your vein. They’ll tunnel the other end under your skin and out of the exit site. Tunneling your CVC under your skin will help keep it from moving.
After your CVC is in place, your doctor will close the insertion site. They will use either Dermabond® (surgical glue) or Steri-Strips™ (surgical tape). They’ll close the exit site with sutures (stitches).
Your doctor will also stitch your CVC to your skin at the exit site. This will help it stay in place until it becomes anchored in the tunnel under your skin. Then, they’ll put on a dressing over your insertion site and a dressing over your exit site and CVC.
After your procedure
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your procedure. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth.
As soon as you’re settled, a nurse will bring your visitors in to be with you.
Once you’re fully awake, they’ll give you a drink and a light snack.
Your nurse will teach you and your caregiver how to care for your dressing before you’re discharged from the hospital. They’ll also give you an emergency kit. The emergency kit should have:
- 2 toothless clamps.
- 1 dressing change kit.
- Alcohol pads.
- Medical (paper) tape.
- Your doctor’s office and emergency telephone numbers.
Keep your emergency kit with you at all times. You’ll need it if:
- Your catheter is leaking.
- Your dressing gets dirty or comes off.
- Your needleless connector or disinfection cap falls off.
Caring for your incisions
You may have some discomfort around your incisions. Your care team will make a plan to manage your pain based on your needs. Tell them if your pain isn’t managed.
It’s important to keep your dressings dry for the first 24 hours (1 day) after your procedure. After 24 hours, you’ll need to change your dressings. Read the section “Changing Your Dressing, Needleless Connectors, and Disinfection Caps” to learn more.
You can take off the dressing over your insertion site 2 days after your procedure. You don’t need to put on a new one. If you have Steri-Strips, leave them in place until they start to peel off. This should happen about 3 to 5 days after your procedure. Do not take off the dressing covering your CVC.
Your healthcare provider will give you instructions about what exercises and movements you can do while your incisions are healing. Check with them before starting heavy exercises, such as running, jogging, or lifting weights.
Caring for your CVC
- Do not put your CVC underwater, such as in a bathtub or swimming pool.
- Clamp the lumens when your CVC isn’t in use.
- Always keep your CVC secure to avoid pulling it. Ask your nurse about the best way to secure your CVC.
- Avoid contact sports and activities that might pull on your CVC, such as football, soccer, and roughhousing. Ask your healthcare provider about any activities before you start them. Be careful not to pull on your CVC when you’re changing your clothes.
-
Check your exit site every day for:
- Redness
- Tenderness
- Leakage
- Swelling
- Bleeding
If you have any of these, call your healthcare provider. You might have an infection.
What to do if your CVC is leaking
- Clamp your CVC above the leak. Move the white clamp on the tubing so it’s above the leak, if you can. If you cannot use the white clamp, use a toothless clamp from your emergency kit.
- Wipe the area that’s leaking with an alcohol pad.
- Cover the area that’s leaking with medical tape.
- Call your healthcare provider right away. CVCs can often be repaired.
What to do if your CVC dressing is damaged, loose, dirty, or wet
Call the doctor’s office right away and follow their instructions. If your nurse taught you to do a dressing change, you may change the dressing as soon as possible. Follow the steps in the “What to do if your needleless connector gets dirty or falls off” section of this resource.
What to do if your needleless connector gets dirty or falls off
If your needleless connector gets dirty, change it. Follow the instructions in the section “How to change your needleless connectors and disinfection caps.”
If your needleless connector falls off, throw it away. Do not put it back on the lumen. Put on a new needleless connector following the steps below.
-
Gather your supplies. You’ll need:
- 2 alcohol pads
- A new needleless connector
- A new disinfection cap
- Make sure the clamp on the lumen is closed.
- Using an alcohol pad, hold the lumen with your nondominant hand close to, but not touching, the needleless connector. Your nondominant hand is the hand you don’t write with.
- Pick up another alcohol pad in your dominant hand. Use the alcohol pad to scrub the end of the lumen for 15 seconds. Throw away the alcohol pad. Let the lumen dry for 15 seconds.
- Pick up the new needleless connector with your dominant hand. If it has a cover, remove the cover. Twist the new needleless connector onto the lumen.
- Put a disinfection cap on the end of the needleless connector.
Call your healthcare provider after you put on the new needleless connector. You may need to have blood drawn to make sure you don’t have an infection.
What to do if your disinfection cap falls off
If your disinfection cap falls off, throw it away. Do not put it back on the lumen.
To put on a new disinfection cap:
- Clean your hands with soap and water or an alcohol-based hand sanitizer.
- Get a new disinfection cap from your emergency kit. Remove the cap from the strip.
- Hold the needleless connector in one hand. With your other hand, gently push and twist the new disinfection cap onto the end of the needleless connector.
Guidelines for showering
Follow the instructions in this section when you shower. Do not put your CVC underwater, such as in a bathtub or swimming pool.
Watch Showering While You Have a Central Venous Catheter (CVC) to learn more.
Use a waterproof cover
You can shower with your catheter in place. Use a single-use waterproof cover that goes over your dressing, such as AquaGuard®. You can buy waterproof covers online.
Each time you shower, cover your dressing and CVC completely with a new waterproof cover to keep them from getting wet. To put on the waterproof cover:
- Peel off the top and side strips.
- Place the top edge above your dressing. Do not let the tape on the waterproof cover touch your dressing. It can lift your dressing when you remove the waterproof cover after showering. Smooth the cover down over your dressing.
- Peel off the bottom strip. Make sure the bottom edge of the waterproof cover is below your dressing. Tuck the lumens of your catheter into the waterproof cover so they’re completely covered. Smooth the bottom edge down.
Do not shower for longer than 15 minutes. Use warm water, not hot water. This will help keep the waterproof cover from coming off.
After your shower, dry the waterproof covering before taking it off. If your dressing gets wet, change it. Follow the instructions in the section “Changing Your Dressing, Needleless Connectors, and Disinfection Caps.”
Use a 4% chlorhexidine gluconate (CHG) solution antiseptic skin cleanser such as Hibiclens®
While your CVC is in place, it’s very important to keep your skin clean. This helps lower your risk of infection. Wash with 4% CHG solution every day while you have a CVC.
CHG is a strong antiseptic that kills germs for up to 24 hours after you use it. Antiseptic is liquid used to kill germs and bacteria. Showering with a 4% CHG solution antiseptic skin cleanser will help lower your risk of infection while you have a CVC.
You can buy a 4% CHG solution antiseptic skin cleanser without a prescription from any local pharmacy or online. You’ll also get a small bottle when you’re discharged from the hospital.
Instructions for using 4% CHG solution
- Wash your hair with your usual shampoo and conditioner. Rinse your head well.
- Wash your face and genital (groin) area with your usual soap. Rinse your body well with warm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Do not put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne after your shower.
Things to remember when using 4% CHG solution
- Do not use CHG on children younger than 2 months old.
- Do not use regular soap, lotion, cream, powder, or deodorant after washing with 4% CHG solution without talking with your nurse first. If you’re in the hospital, your nurse might give you a lotion you can use after using 4% CHG solution.
- Do not use 4% CHG solution on your head, face, ears, eyes, mouth, genital area, or on deep wounds. If you have a wound and aren’t sure if you should use 4% CHG solution on it, ask your healthcare provider.
- Do not use 4% CHG solution if you’re allergic to chlorhexidine.
- Stop using 4% CHG solution if your skin gets irritated, or you have an allergic reaction when using it. If this happens, call your healthcare provider.
How to flush your CVC
A member of your care team may tell you if you need to flush your CVC. If you do, follow the steps below. Most people will not need to flush their lines at home.
Supplies
- 10 mL syringe(s) prefilled with normal saline solution. You’ll need 1 syringe for each lumen.
- Nonsterile gloves
- 2 alcohol pads for each lumen
- 1 disinfection cap for each lumen
Steps to flushing your CVC
- Gather your supplies.
-
Clean your hands well.
- If you’re washing your hands with soap and water, wet your hands with warm water and apply antibacterial soap. Rub your hands together well for at least 20 seconds, then rinse. Dry your hands with a paper towel and use that same towel to turn off the faucet. If you don’t have paper towels, it’s OK to use clean cloth towels. Replace them when they’re wet.
- If you’re using hand sanitizer, be sure to cover all of your hands with it. Rub them together until they’re dry.
- Put on a pair of nonsterile gloves.
-
Release the air bubbles in the syringe. To do this:
- Hold the syringe so the tip is pointing upward.
- Gently tap the side. The air bubbles should rise to the top.
- Loosen but don’t remove the cap on the syringe.
- Press the plunger on the syringe until the air is pushed out.
- Retighten the cap.
- Pick up 1 lumen in your nondominant hand. If you have a disinfection cap, remove it. Using your dominant hand, scrub the end of the needleless connector with an alcohol pad for 15 seconds. Let it dry for 15 seconds.
- Remove the cap from the syringe. move the cap from the syringe. Throw away the cap. Keep holding the lumen away from your body. Make sure nothing touches the clean end of the needleless connector while you’re doing this.
- Carefully push the syringe into the needleless connector. Twist the syringe clockwise (to the right) until the connection feels secure.
- Unclamp the lumen. Before starting to inject the saline, make sure there aren’t any twists or other blockages in the tubing.
- Use the push/pause method to flush your CVC.
- Quickly inject ⅓ of the saline. Pause.
- Inject another ⅓ of the saline. Pause.
- Inject the last ⅓ of the saline.
If you cannot inject the saline, stop and check that the lumen is unclamped. Make sure there are no twists or other blockages in the tubing. Try to inject the saline again.
If you still cannot inject the saline, do not use extra pressure to flush the line. Follow steps 10 to 12 and then call your healthcare provider.
- Re-clamp the lumen.
- Turn the syringe counterclockwise (to the left) to disconnect it from the lumen. Throw it away.
- Attach a new disinfection cap to the end of the needleless connector.
Repeat steps 4 to 12 for each lumen. Once you’re done, throw away your mask and gloves. Wash your hands well with warm water and antibacterial soap or use hand sanitizer.
When to call your healthcare provider
Call your healthcare provider right away if:
- There’s redness, swelling, or drainage around your exit site.
- You have a fever of 100.4 °F (38 °C) or higher.
- Your catheter is broken or leaking.
- Your needleless connector falls off.
- There’s blood backing up into your catheter.
- Your catheter gets disconnected from your pump.
- Your catheter is connected to a pump and the alarm on the pump is going off.
- You have an unexplained problem with your catheter.