This information will help you get ready for your procedure to have prostate fiducial markers and a rectal spacer placed. You’ll have this procedure before you start your prostate radiation therapy.
About your prostate
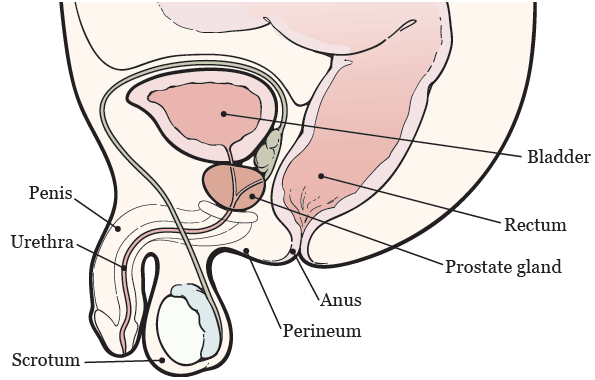
Your prostate is a walnut-sized gland located below your bladder, directly in front of your rectum (see Figure 1). It surrounds your urethra, which is the tube that drains urine from your bladder. Your prostate adds fluid to your semen.
About fiducial markers and rectal spacers
Fiducial markers are tiny metal objects (about the size of a grain of rice). They help your healthcare providers line up the beams of radiation and make sure your radiation therapy is delivered exactly the same way each time. This helps them target the tumor and avoid your nearby healthy tissue. The fiducial markers will stay in your prostate after your treatment.
You’ll get a rectal spacer called SpaceOAR™ hydrogel. It is a gel that’s placed between your prostate and rectum to move your rectum away from your prostate. This protects your rectum from radiation and reduces some side effects of radiation therapy. The rectal spacer will stay in place for 3 months. Then, it’ll be absorbed by your body and come out in your urine.
Before your procedure
Tell your healthcare provider if you:
- Take an anticoagulant (blood thinner). Read the section “Ask about your medicines” for examples.
- Take any steroid medicines (such as prednisone).
- Take any dietary supplements (such as vitamins, herbal supplements, or natural or home remedies).
- Have taken any antibiotics in the past 3 months.
- Have any heart condition.
- Have any implanted devices (such as knee or hip replacements).
- Are allergic to the antibiotic ciprofloxacin (Cipro®) or any other medicines.
- Are allergic to latex.
- Have had a urinary tract infection (UTI) in the last month.
- Have ever had an infection or been hospitalized after a prostate biopsy.
- Have had Achilles tendon injuries or tendonitis (inflammation of your tendons).
- Have trouble hearing.
- Work in a hospital or nursing home.
Ask about your medicines
You may need to stop taking some of your medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking. We’ve included some common examples below.
Anticoagulants (blood thinners)
If you take a blood thinner (medicine that affects the way your blood clots), ask the healthcare provider doing your procedure what to do. They may or may not tell you to stop taking the medicine, depending on the reason you’re taking it.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It has important information about medicines you might need to stop taking before your procedure and what medicines you can take instead.
Pain medicines and antianxiety medicines
Tell your healthcare provider if you’re taking any pain medicines or antianxiety medicines. It’s important to keep taking these medicines on schedule, even during your treatment. You may be able to take them on the morning of your procedure, if needed.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Fill out a Health Care Proxy form
If you have not already filled out a Health Care Proxy form, we recommend you do now. If you already filled one out or have any other advance directives, bring them to your next appointment.
A health care proxy is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent.
- To learn about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn about being a health care agent, read How to Be a Health Care Agent.
Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
Get your supplies
You’ll need to get the following supplies:
- 2 saline enemas (such as Fleet® saline enemas). You can buy these at your local pharmacy without a prescription.
- Ciprofloxacin (Cipro®) 500 milligram (mg) tablets. This is an antibiotic (medicine to help prevent an infection). Your healthcare provider will give you a prescription before your procedure.
The day before your procedure
If you have any changes in your health or need to cancel your procedure for any reason, call your primary radiation oncologist.
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-7606.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
Give yourself a saline enema
Give yourself a saline enema 2 hours before you go to bed. Follow the instructions in the package.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
The day of your procedure
If your healthcare provider told you to take certain medicines the morning of your procedure, take only those medicines with a small sip of water.
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Shower
The morning of your procedure, shower like usual. Do not put anything on your skin after your shower. This includes lotion, cream, deodorant, makeup, powder, perfume, and cologne.
Give yourself a saline enema
Give yourself a saline enema 3 hours before your procedure is scheduled to start. Follow the instructions in the package.
Things to remember
- Do not wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Leave valuable items (such as credit cards and jewelry) at home.
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during your procedure can damage your eyes. If you do not have glasses, bring a case for your contacts.
- If you wear dentures, you can wear them until you’re in the operating room. Make sure to tell the operating room staff that you’re wearing them before you fall asleep for your procedure.
What to expect
Once you arrive at the hospital, doctors, nurses, and other staff members will ask you to say and spell your name and date of birth many times. This is for your safety. People with the same or similar name may be having a procedure on the same day.
When it’s time for your procedure, you’ll change into a hospital gown. A nurse will place an intravenous (IV) line into one of your veins, usually in your hand or arm. Then, a staff member will bring you to the operating room. Once you’re comfortable, you’ll get anesthesia (medicine to make you sleep during a surgery or procedure) through your IV.
Once you’re asleep, your healthcare provider will use rectal ultrasound to see your prostate. They’ll put tiny needles into your prostate through your perineum (the area of skin between your scrotum and anus). They’ll place 3 fiducial markers into your prostate through the needles, then remove the needles. After that, they’ll use another needle to inject the rectal spacer gel into the space between your prostate and rectum.
After your procedure
In the hospital
When you wake up, you’ll be in the Post Anesthesia Care Unit (PACU). You’ll stay there until you’re fully awake and can urinate (pee) without any trouble. A nurse will talk with you and your caregiver and give you your discharge instructions.
At home
You might have a feeling of fullness in your rectum for the 2 days after your procedure. This is normal and will not affect your bowel movements.
Do not put anything in your rectum for 3 months after your procedure. If your healthcare provider tells you to give yourself an enema before any of your radiation treatments, it’s OK to do so.
Medicine instructions
Take 1 (500 mg) tablet of ciprofloxacin before you go to bed after your procedure. Keep taking 1 (500 mg) tablet every 12 hours for 3 days. This will help prevent an infection in your prostate.
If you have any pain, you can take an over-the-counter (not prescription) pain medicine, such as acetaminophen (Tylenol®) or ibuprofen (Advil®, Motrin®).
Physical activity and exercise
You can drive and do your normal activities 24 hours after your procedure. Do not lift anything heavier than 10 pounds (4.5 kilograms) for 1 week after your procedure.
Eating and drinking
You can go back to your usual diet right away after your procedure.
When to call your healthcare provider
Call your healthcare provider right away if you have:
- Increasing pain or pain that does not get better after taking over-the-counter pain medicine
- A fever of 100.4 °F (38 °C) or higher
- Chills
- Trouble urinating
- Blood in your stool (poop) or urine (pee)
- Dizziness
Helpful phone numbers
Anesthesia
212-639-6840
Call with questions about anesthesia.
Bobst International Center
888-675-7722
MSK welcomes patients from around the world. If you’re an international patient, call for help coordinating your care.
Patient Billing
646-227-3378
Call Patient Billing with any questions about preauthorization with your insurance company. This is also called preapproval.
Patient Representative Office
212-639-7202
Call with questions about the Health Care Proxy form or if you have concerns about your care.
Instructions before and after your procedure
A staff member will call you after the day before your procedure to confirm the time of your procedure and any other logistics. Below is a summary of what to do before and after your procedure.
Before your procedure
| Instructions | Purpose | |
|---|---|---|
| Food |
| For bowel preparation |
| Drinks |
| |
| Saline enema |
| |
| Medicines |
|
After your procedure
| Instructions | Purpose | |
|---|---|---|
| Antibiotics |
| To prevent a prostate infection |
| Food and drink |
| To make sure your rectum is empty and your bladder is comfortably full during your radiation treatments |