This guide will help you get ready for your pelvic surgery for DSRCTs at MSK Kids. It will also help you know what to expect as you recover.
Use this guide as a source of information in the days leading up to your surgery. Bring it with you on the day of your surgery. You and your care team will use it as you learn more about your recovery.
In this resource, the words “you” and “your” refer to you or your child.
About your pelvic surgery for DSRCTs
DSRCTs are a type of sarcoma. DSRCTs most often start in your abdomen (belly). They’re often in your peritoneum (PAYR-ih-toh-NEE-um), the tissue that lines the inside of your abdomen and pelvis. Your peritoneum also covers most of the organs in your abdomen.
DSRCTs can also spread to other nearby organs, such as your bladder, colon, and liver.
The standard treatment for DSRCTs is surgery, chemotherapy (chemo), and radiation therapy. At MSK, most people have 3 separate surgeries to treat DSRCT.
- The first surgery is to take out tumors in your abdomen.
-
The second surgery is to take out tumors in your pelvis.
- Your surgeon may also give you a temporary ileostomy (IL-ee-OS-toh-mee) during this surgery. An ileostomy is a small opening in your abdomen where your bowel movements (poop) can leave your body. Your ileostomy will keep your bowel movements from passing through your colon (large intestine) and rectum. This lets the area heal after your surgery.
-
The third surgery is to reverse your ileostomy, if you have one. That means your bowel movements will go back to passing through your colon and rectum like normal.
- Some people have intraperitoneal (IN-truh-PAYR-ih-toh-NEE-ul) chemo as part of their DSRCT treatment. Your surgeon will also place an intraperitoneal catheter (IP catheter) in your abdomen during this surgery. An IP catheter is a thin, flexible tube that goes from outside your body into your peritoneal (PAYR-ih-toh-NEE-ul) cavity. This is the space between the tissue lining your abdomen and pelvis, and the tissue covering organs in your abdomen.
What will happen during my pelvic surgery for DSRCTs?
Pelvic surgery for DSRCT can be done in different ways. Depending on how your surgery is done, your surgeon will make 1 or more incisions (surgical cuts) in your abdomen.
- When your surgeon makes 1 long incision on your abdomen, it’s called open surgery. Your surgeon will take out any tumors through this incision.
- When your surgeon makes several small incisions on your abdomen, it’s called minimally invasive surgery. Your surgeon will put small surgical tools and a video camera into the incisions to take out any tumors. Some surgeons use a robotic device to help guide the video camera and surgical tools.
Your surgeon may need to take out part of your colon or rectum during your surgery. If they do, they may give you a temporary ileostomy (IL-ee-OS-toh-mee). Read the section “About ileostomies” to learn more.
Your surgeon and other members of your care team will talk with you about what to expect before, during, and after your surgery. They’ll go into detail about the plan for your surgery and answer any questions you have.
Your surgeon will often know before your surgery if you’ll need a temporary ileostomy. But they’ll make the final decision during your surgery.
About ileostomies
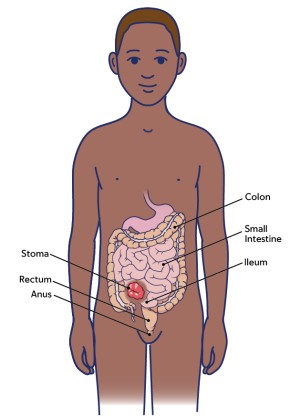
An ileostomy is a small opening in your abdomen where your bowel movements can leave your body (see Figure 1). The ileostomy will keep your bowel movements from passing through your colon and rectum. This lets the area heal after your surgery.
The part of your intestine that’s outside your body is called a stoma. Your stoma will be pink or red and look shiny and moist. Bowel movements and gas leave your body through your stoma and go into a plastic pouch that covers your stoma. It’s normal for the bowel movements to be more liquid than usual.
You may have had a temporary ileostomy. If so, a wound, ostomy, and continence (WOC) nurse will help teach you how to care for it before and after your surgery.
Your surgeon will close your ileostomy after a few months. Very few people need a permanent ileostomy.
Before your pelvic surgery for DSRCTs
This section will help you get ready for your surgery. Read it when your surgery is scheduled. Refer to it as your surgery gets closer. It has important information about what to do to get ready.
As you read this section, write down questions to ask your healthcare provider.
Getting ready for your surgery
You and your care team will work together to get ready for your surgery. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
You may need to follow special instructions before surgery based on the medicines and supplements you take. If you do not follow those instructions, your surgery may be delayed or canceled.
-
I take any prescription medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. Examples include:
- Medicines you swallow.
- Medicines you take as an injection (shot).
- Medicines you inhale (breathe in).
- Medicines you put on your skin as a patch or cream.
- I take any over-the-counter medicines, including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take any dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to make you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I use recreational drugs, such as marijuana.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your surgery. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medicine to help prevent them.
Here are things you can do before your surgery to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
-
Try to stop drinking alcohol once your surgery is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
These are early signs of alcohol withdrawal and can be treated.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and surgery. All your medical information will be kept private, as always.
About smoking
If you smoke or use an electronic smoking device, you can have breathing problems when you have surgery. Vapes and e-cigarettes are examples of electronic smoking devices. Stopping for even a few days before surgery can help prevent breathing problems during and after surgery.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after surgery. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your surgery.
Using MSK MyChart
MSK MyChart (mskmychart.mskcc.org) is MSK’s patient portal. You can use it to send and read messages from your care team, view your test results, see your appointment dates and times, and more. You can also invite your caregiver to make their own account so they can see information about your care.
If you do not have an MSK MyChart account, you can sign up at mskmychart.mskcc.org. You can also ask a member of your care team to send you an invitation.
If you need help with your account, call the MSK MyChart Help Desk at 646-227-2593. They are available Monday through Friday between and (Eastern time).
About your Goals to Discharge Checklist
After your surgery, you’ll focus on getting well enough to leave the hospital. We’ll send a Goals to Discharge Checklist to your MSK MyChart account to help you track how you’re doing.
You can use your Goals to Discharge Checklist to see the goals you need to meet before leaving the hospital. You can also update your progress throughout the day. Your updates send alerts to your surgical team about your progress.
To learn more, read Frequently Asked Questions About the Goals to Discharge Checklist.
About Enhanced Recovery After Surgery (ERAS)
ERAS is a program to help you get better faster after your surgery. It’s important to do certain things before and after your surgery as part of the ERAS program.
Before your surgery, make sure you’re ready by:
- Reading this guide. It will help you know what to expect before, during, and after your surgery. If you have questions, write them down. You can ask your healthcare provider at your next visit or call their office.
- Exercising and following a healthy diet. This will help get your body ready for your surgery.
After your surgery, help yourself recover more quickly by:
- Starting to move around as soon as you can. The sooner you get out of bed and walk, the quicker you can get back to your usual activities.
- Exercising your lungs. Use your incentive spirometer or pinwheel to help your lungs expend fully. This helps prevent pneumonia (lung infections).
- Exercising your body. Your PT and OT will teach you activities and exercises to help you get stronger.
Presurgical testing
You’ll have a presurgical testing (PST) or pediatric presurgical testing (PPST) appointment before your surgery. You’ll get a reminder from your surgeon’s office with the appointment date, time, and location.
You can eat and take your usual medicine(s) the day of your appointment.
It’s helpful to bring these things to your appointment:
- All the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with advance practice provider (APP) during your appointment. They work closely with your surgical team.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm
- A chest X-ray
- Blood tests
Your APP may recommend that you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your surgery.
Meet with a Wound, Ostomy, Continence (WOC) nurse
If you’ll have a temporary ileostomy, you’ll meet with a WOC nurse before your surgery. A WOC nurse is a registered nurse with special training in wound and ostomy care. They’ll teach you and your family how to care for your new colostomy and help you become more independent. A WOC nurse will also show you a colostomy pouch so you can get familiar with it.
The Pediatric Pain and Palliative Care Team (PACT)
The PACT is a team of doctors and APPs. We support children and families facing serious illnesses at MSK Kids.
The goal of palliative care is to help you and your family during your treatment. The PACT can help with physical, mental, social, and spiritual challenges. We can help no matter your age or the stage of your illness. We can also help no matter if you’re getting care in the hospital or as an outpatient. Palliative care is important and helpful for everyone.
The PACT respects your choices, values, and beliefs. We encourage you and your family to be active in making decisions about your goals and plans of care. We’ll work together with all members of your care team. Our goal is to make sure you and your family have the support you need to live as well as possible.
Integrative Medicine
MSK’s Integrative Medicine and Wellness Service offers help with relaxing, easing discomfort, and improving your overall well-being. Our specialists are trained and certified in integrative health practices such as:
- Massage therapy
- Music therapy
- Dance therapy
- Yoga
- Meditation
- Mind-body fitness
- Acupuncture
You’ll talk with an Integrative Medicine Specialist during your first Integrative Medicine and Wellness visit. They’ll tell you about the integrative medicine and wellness services available at MSK. They’ll also talk with you about:
- Different types of integrative medicine and holistic techniques.
- How to make use of these therapies during your stay.
- How they can help you and your family before surgery and during recovery.
Help your body get ready for surgery
You can recover faster and easier if you help your body be in its best shape for your surgery. This section has examples of things you can do to get your body ready for surgery. Your care team will help you decide which activities are best for you.
Practice breathing and coughing
Practice taking deep breaths and coughing before your surgery. You can do this by:
- Walking around or playing.
- Blowing bubbles or blowing a tissue in the air.
- Using your incentive spirometer, if your care team gave you one.
Move around and be active
Try to do physical activity every day. Examples include walking, swimming, or biking. MSK also offers free virtual classes for all ages that can help you be active. Ask your healthcare provider for more information.
Practice meditation and mindfulness
Mindful breathing, meditation, yoga, movement practice, massage, and acupressure techniques can support you as you get ready for surgery.
Our Integrative Medicine and Wellness Service videos can help you find the right activities to add to your routines before surgery. Visit www.msk.org/integrative-medicine-multimedia to find the videos. You can also visit www.msk.org/meditation to see guided meditation videos made by our expert mind-body specialists.
Follow a healthy diet
An MSK Kids clinical dietitian nutritionist can talk with you about how to get ready for surgery. You can learn how to make sure your nutrition is the best it can be.
If you’re getting other cancer treatments before your surgery, they can cause taste changes, appetite loss, and trouble digesting food. This can make it hard to eat enough food, which can lead to weight loss. Your outpatient MSK Kids clinical dietitian nutritionist can work with you to make a plan that helps with eating challenges.
It’s also helpful to follow these general guidelines:
- Have small, frequent meals. For example, have a half-sized meal every 2 to 3 hours. Aim for 6 to 8 small meals a day instead of 3 large meals.
- Make and follow a meal schedule. Don’t wait to eat until you’re hungry. Put the schedule in a place for everyone to see.
- Keep your favorite go-to foods in your home where you can get to them easily.
- Buy single-serving food items that you can eat easily, such as drinkable yogurt smoothies or cheese sticks.
-
Cook in batches so you have leftovers.
- Keep 1 extra serving in your refrigerator for the next day, but not longer.
- Freeze the other extra servings. When you’re ready to use a serving, thaw it in the refrigerator or microwave, not on the kitchen counter. Then reheat it until it’s steaming hot.
- Include many different food groups and food types in your diet, unless your doctor or clinical dietitian nutritionist tells you not to.
- Sometimes drinking is easier than eating. Try getting more calories from liquids than solid foods. For example, have milkshakes or nutritional supplements such as PediaSure® or Carnation Breakfast Essentials®.
- Keep your dining experience enjoyable, with no stress. Try having family mealtimes or group snack times with family.
- Think of your nutrition as being just as important as your medicines.
Remember to choose foods that are high in calories and protein. Talk with your MSK Kids clinical dietitian nutritionist about foods that work best based on what you like or your meal patterns.
Have a carbohydrate drink the night before or morning of your surgery
One of your healthcare providers will give you a bottle of CF(Preop)® or Ensure® Pre-Surgery to drink the night before or morning of your surgery. These are carbohydrate drinks that make fasting (not eating) before surgery less stressful for your body. This helps you heal and recover better after surgery.
Meet with other healthcare professionals, if needed
MSK has many different healthcare professionals who can help you before, during, and after your cancer treatment.
- Social workers can help you cope with the emotional, social, and physical effects of a cancer diagnosis. Our social workers provide counseling and practical assistance. They help families cope with their child’s disease, improve communication with family and friends, share information on community resources, and help adjust to medical treatment.
- Child life specialists are trained professionals who are experts in human growth and development. If you’re worried or stressed about your procedure, they can help you plan ways to be more comfortable and relaxed. MSK’s child life specialists have a variety of backgrounds and interests, including education, psychology, fine arts, and art therapy. Together, our skills and certifications offer a full range of child life services that educate and empower patients and their families during an illness.
- Counselors and therapists can meet with you and your family members and provide counseling for emotional problems related to coping with cancer. MSK’s counseling center also has support groups that meet regularly.
Your healthcare provider may offer you a referral to these services. You can also ask for a referral if you’re interested.
Talk with your social worker about housing, if needed
The Ronald McDonald House provides temporary housing for out-of-town pediatric cancer patients and their families.
MSK also has arrangements with several local hotels and housing facilities that may give you a special lower rate. Your social worker can talk with you about your options and help you make reservations. You can also call 212-639-8315 to talk with the Pediatric Patient Services Coordinator.
Fill out a Health Care Proxy form, if needed
If you’re age 18 or older and have not already filled out a Health Care Proxy form, we recommend you do now. If you already filled one out or have any other advance directives, bring them to your next appointment.
A health care proxy is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent.
- To learn about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn about being a health care agent, read How to Be a Health Care Agent.
Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
Get your bowel prep supplies
You will need to do a bowel preparation (bowel prep) before your surgery. You’ll need these supplies:
- Polyethylene glycol (MiraLAX®) powder
- Clear liquids that are not red, orange, or purple
Make sure to get enough clear liquids to have while you’re following a clear liquid diet.
Your healthcare provider will also give you a prescription for the medicines below. Make sure you have them before you start your bowel prep.
- Metronidazole
- Neomycin
7 days before your surgery
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your surgery. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your surgery. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment.
Have imaging scans, if needed
You’ll need to have imaging scans to help your healthcare providers plan your surgery. If you have them done somewhere other than MSK, your healthcare provider may ask you to bring the disc with copies of the imaging scans to one of your appointments.
2 days before your surgery
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your surgery. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
1 day before your surgery
Get the MiraLAX mixture ready
Mix MiraLAX with a clear liquid in the morning the day before your surgery. Your care team will tell you how much MiraLAX powder and liquid to use.
Stir the mixture until the MiraLAX powder dissolves. Once the MiraLAX dissolves, you can put the mixture in the refrigerator.
Start following a clear liquid diet at noon (12 p.m.)
Start following a clear liquid diet at noon (12 p.m.) the day before your surgery.
A clear liquid diet includes only liquids you can see through. You can find examples in the “Clear liquid diet” table. Avoid clear liquids that are red, orange, or purple.
While you’re following a clear liquid diet:
- Do not eat any solid foods.
- Drink different types of clear liquids. Do not just drink water, coffee, and tea. This helps make sure you get enough calories and is an important part of your bowel prep.
- Do not drink any liquids you cannot see through, such as milk or smoothies.
- Do not drink sugar-free liquids unless you have diabetes and your healthcare provider tells you to.
Clear liquid diet
| OK to have | Do not have | |
|---|---|---|
| Soups |
|
|
| Sweets |
|
|
| Drinks |
|
|
Start drinking the MiraLAX mixture at 2 p.m.
Start drinking the MiraLAX mixture at the day before your surgery.
Drink the MiraLAX mixture over the next 3 to 4 hours. Aim to finish between and
The MiraLAX will make you have bowel movements often. Make sure you’re near a bathroom once you start taking it.
Having lots of bowel movements can irritate (bother) your anus (where your poop leaves your body). Putting petroleum jelly (Vaseline®) or A & D® ointment on the skin around your anus after each bowel movement can help.
Note the time of your surgery
A staff member from the Admitting Office will call you after the day before your surgery. If your surgery is scheduled for a Monday, they’ll call you on the Friday before. If you don’t get a call by , call 212-639-7002.
The staff member will tell you what time to arrive at the hospital for your surgery. They’ll also remind you where to go. Visit www.msk.org/locations for information about MSK’s locations, including directions and parking.
Take neomycin and metronidazole at 6 p.m. and 10 p.m.
Take 1 dose of neomycin and 1 dose of metronidazole at the night before your surgery.
Take another dose of neomycin and another dose of metronidazole at the night before your surgery.
Shower or bathe with a 4% CHG solution antiseptic skin cleanser, such as Hibiclens
4% CHG solution is a skin cleanser that kills germs for 24 hours after you use it. Showering with it before your surgery will help lower your risk of infection after surgery. We will give you a bottle during your PST appointment. You can also buy it at your local pharmacy without a prescription.
Shower or bathe with 4% CHG solution the night before or morning of your surgery.
- Wash your hair with your usual shampoo and conditioner. Rinse your head well.
- Wash your face and genital (groin) area with your usual soap. Rinse your body well with warm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Do not put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne after your shower.
The morning of your surgery
You can keep drinking clear liquids between midnight (12 a.m.) and 2 hours before your scheduled arrival time. How much you can have depends on your age. Follow the instructions below.
- Ages 0 to 3: You can drink up to 4 ounces (120 milliliters) of clear liquids between midnight and 2 hours before your scheduled arrival time.
- Ages 4 to 8: You can drink up to 6 ounces (180 milliliters) of clear liquids between midnight and 2 hours before your scheduled arrival time.
- Ages 9 to 13: You can drink up to 8 ounces (240 milliliters) of clear liquids between midnight and 2 hours before your scheduled arrival time.
- Ages 13 and older: You can drink up to 12 ounces (360 milliliters) of clear liquids between midnight and 2 hours before your scheduled arrival time.
| Do not drink anything starting 2 hours before your scheduled arrival time. This includes water and other clear liquids. |
Take your medicines as instructed
A member of your care team will tell you which medicines to take the morning of your surgery. Take only those medicines with a sip of water. Depending on what you usually take, this may be all, some, or none of your usual morning medicines.
Things to remember
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during surgery can damage your eyes.
- Do not wear any metal objects. Take off all jewelry, including body piercings. The tools used during your surgery can cause burns if they touch metal.
- Do not wear any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Leave valuable items at home.
- If you’re menstruating (have your monthly period), use a sanitary pad, not a tampon. We’ll give you disposable underwear and a pad if you need them.
What to bring
- 1 comfort item, such as a blanket or stuffed animal.
- 1 or 2 portable electronic devices, such as a smartphone or tablet. Don’t forget their charger.
- All the medicines you’re taking, including prescription and over-the-counter medicines, supplements, patches, and creams.
- Your incentive spirometer, if you have one.
- Your Health Care Proxy form and other advance directives, if you filled them out.
- This guide. You’ll use it to learn how to care for yourself after surgery.
Once you’re in the hospital
When you get to the hospital, take the B elevator to the 6th floor. Check in at the desk in the PSC waiting room.
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or a similar name may be having surgery on the same day.
We’ll give you a hospital gown, robe, and nonskid socks to wear when it’s time to change for surgery.
Meet with a nurse
You’ll meet with a nurse before surgery. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches, and creams.
If you have an implanted port or central venous catheter (CVC), the nurse will access it. If you don’t, your anesthesiologist (A-nes-THEE-zee-AH-loh-jist) will place an intravenous (IV) line in one of your veins in the operating room. An anesthesiologist is a doctor with special training in using anesthesia during your surgery.
Meet with an anesthesiologist
You’ll also meet with an anesthesiologist before surgery. They will:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your surgery.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Your care team may talk with you about placing an epidural catheter or peripheral nerve catheter (nerve block) during your surgery. These are thin, flexible tubes that carry medicine to block a group of nerves from feeling pain. They’re another way to help manage pain after your surgery.
Get ready for surgery
When it’s time for your surgery, you’ll either walk into the operating room or a staff member will bring you there on a stretcher. A member of the operating room team will help you onto the operating bed.
Once you’re comfortable, your anesthesiologist will give you anesthesia and you’ll fall asleep. You’ll also get fluids through your implanted port, CVC, or IV line during and after your surgery.
During your surgery
After you’re fully asleep, your surgery team will place a breathing tube through your mouth into your airway. It will help you breathe. They’ll also place a urinary (Foley) catheter in your bladder. It will drain your urine (pee) during your surgery.
Once your surgery is finished, your surgery team will close your incisions up to the skin. They will place a special dressing called a wound vac over the open skin. Then, they’ll cover the wound vac with a normal bandage.
After your pelvic surgery for DSRCTs
This section will help you know what to expect after your surgery. You’ll learn how to safely recover from your surgery both in the hospital and at home.
As you read this section, write down questions to ask your healthcare provider.
In the Pediatric Intensive Care Unit (PICU), Intensive Care Unit (ICU), or Post-Anesthesia Care Unit (PACU)
You’ll be in the PICU, ICU, or PACU when you wake up after your surgery. Before your surgery, your care team will talk with you about what to expect when you wake up.
A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may still have a breathing tube. If you don’t, you’ll be getting oxygen through a thin tube that rests below your nose or a mask that covers your nose and mouth.
Pain medicine
Right after your surgery, you’ll get IV pain medicine through your implanted port, CVC, or IV line. You may also get pain medicine through an epidural catheter or nerve block. Tell one of your healthcare providers if your pain isn’t managed.
You’ll be able to control your pain medicine using a button called a patient-controlled analgesia (PCA) device. Read Patient-Controlled Analgesia (PCA) to learn more.
Tubes and drains
You’ll have 1 or more of these tubes and drains after your surgery. Your care team will tell you what to expect.
- 1 to 2 abdominal drains. These are flexible tubes that come out of your incision and are attached to a drainage bag. They will carry liquid from your abdomen.
- A wound vac. This is a special dressing over your incision. It gently pulls air and liquid away from your incision. This can lessen swelling and help it heal.
- A nasogastric (NG) tube. This is a thin, flexible tube that goes through your nose into your stomach. It will drain air and liquid from your stomach.
- A breathing tube. This is a flexible tube that goes through your mouth into your airway. It will help you breathe.
- An arterial line. This is a thin, flexible tube that goes into one of your arteries (blood vessels). It will keep track of your blood pressure.
- A urinary (Foley) catheter. This is a thin, flexible tube that’s put through your urethra into your bladder. It will carry urine from your bladder into a drainage bag. This helps your care team keep track of how much urine you’re making.
Your healthcare providers will care for your tubes and drains while you’re in the hospital. Your care team will keep track of how much liquid is draining from your abdominal drain. Once the amount is low enough, they’ll take it out.
Most people don’t have any tubes or drains by the time they’re ready to leave the hospital. If you will have a tube or drain when you leave, your healthcare providers will teach you how to care for it at home. They’ll also make sure you have the supplies you need.
Physical therapy and occupational therapy
Some people need help moving, walking, doing their usual activities, or doing self-care tasks after surgery. If you do, a physical therapist (PT), occupational therapist (OT), or both may visit you.
- Your PT can help you move and function better after surgery. They’ll help you get back the strength, balance, and coordination you need to do things like crawling, walking, climbing stairs, playing, or doing sports.
- Your OT can help you improve the skills you need to do important everyday activities. They’ll help you if you have trouble with self-care tasks (such as getting dressed and brushing your teeth), play activities, or skills you need for school or work.
Your PT and OT will talk with you about how often you will have physical therapy, occupational therapy, or both. To learn more, read Staying Active Before and After Surgery for Pediatric Patients.
Moving to your hospital room
Most people stay in the PICU, ICU, or PACU for 1 to 2 days. You’ll stay until:
- Your breathing tube and arterial line have been taken out, if you had them.
- You can get out of bed and move around.
- You can do breathing exercises, such as using your incentive spirometer or pinwheel.
- Your vital signs are in an acceptable range.
Once you’re ready, a staff member will take you to your hospital room.
In your hospital room
How long you’re in the hospital after your surgery depends on your recovery and your treatment plan. Your care team will tell you what to expect.
While you’re in the hospital, your care team will teach you how to care for yourself while you’re recovering from your surgery. You will probably meet with a social worker, child life specialist, clinical dietitian nutritionist, and other members of your care team. They will work with each other and with you to help you recover.
You can also help yourself recover more quickly by:
- Starting to move around as soon as you can. The sooner you get out of bed and walk, the quicker you can get back to your normal activities.
- Exercising your lungs. Use your incentive spirometer or pinwheel to help your lungs expend fully. This helps prevent pneumonia (lung infections).
- Exercising your body. Your PT and OT will teach you activities and exercises to help you get stronger.
You can use your Goals to Discharge Checklist to track your progress during your recovery. Read Frequently Asked Questions About the Goals to Discharge Checklist to learn more.
Managing your pain
You’ll have some pain after your surgery. Your healthcare providers will make a pain plan for you so you’re as comfortable as possible.
- You’ll get opioid (also called narcotic) pain medicines for a little while to treat the pain from your surgery. You’ll get the lowest dose and take them for the shortest length of time needed.
- You’ll get a few other types of pain medicines to make sure you’re comfortable and so you can take less of the opioid medicine(s).
- You may get pain medicine through your epidural or nerve block.
The Pediatric Pain and Palliative Care Team (if you’re younger than age 18) or Anesthesia Pain Team (if you’re age 18 or older) and your anesthesiologist will talk with you about your pain plan and answer your questions.
Your healthcare providers will visit you every day. They will ask about your pain and to make sure your pain is as well controlled as possible. If you have pain, tell one of your healthcare providers. It’s important to control your pain so you can do your breathing exercises and move around. Controlling your pain will help you recover better.
You’ll get a prescription for oral pain medicine (pain medicine you swallow) before you leave the hospital. Talk with your healthcare provider about possible side effects and when to start switching to over-the-counter pain medicines. Bring your prescription pain medicine to your follow-up visit in clinic.
Managing pain through integrative medicine
Our Integrative Medicine specialists can support you if you’re having pain after surgery. We can help you practice mindfulness and meditation through breathing exercises, mindful movement, and use of guided imagery. Massage techniques and music therapy may provide comfort. Playfulness through dancing can shift your mood and take your focus off your pain.
If you’re interested in managing pain through integrative medicine, ask a member of your care team for an Integrative Medicine consult.
Moving around and walking
Moving around and walking will help lower your risk for blood clots and pneumonia. It will also help you start passing gas and having bowel movements (pooping) again. You’ll need to have a bowel movement before you’re discharged from the hospital.
You can move around by walking to the sink or bathroom or around the unit. Your nurse, physical therapist, or occupational therapist will help you move around, if needed. Mindful movement therapies, such as dance therapy, tai chi, and yoga, are also available. If you’re interested in mindful movement therapy, ask a member of your care team for an Integrative Medicine consult.
Read Frequently Asked Questions About Walking After Your Surgery to learn more about how walking after surgery can help you recover.
Exercising your lungs
It’s important to exercise your lungs so they expand fully. This helps prevent pneumonia.
- Use your incentive spirometer or pinwheel 10 times every hour you’re awake. Read How To Use Your Incentive Spirometer to learn more.
- Do coughing and deep breathing exercises. A member of your care team will teach you how. It’s best to do these exercises soon after taking your pain medicine. Holding your pillow across your incision while you do them can also help.
One of MSK’s Integrative Medicine providers can also help you exercise your lungs by guiding you through breathing techniques or meditation.
Caring for your temporary ileostomy
If you have a temporary ileostomy, your nurses, WOC nurse, or both will check your stoma every day. You’ll have a pouch in place to collect the stool that comes out of your stoma.
Your WOC nurse will visit you in your hospital room to teach you how to care for your ileostomy. Your case manager will also visit you to help you get supplies to use at home.
To learn more, read Caring for Your Ileostomy or Colostomy.
Eating and drinking
You will not be able to eat or drink anything for a few days after surgery. You will get all the fluids and nutrients you need through your IV line.
Your surgery team will tell you when you can start eating and drinking. At first, you’ll only drink liquids. After that, you’ll slowly start eating solid food as you can take more in.
Once you start eating more solid food, your inpatient MSK Kids dietitian will meet with you. They’ll talk with you about foods to include in your diet after surgery. It’s best to choose foods high in protein so your body has the nutrients it needs to best recover after surgery.
Managing bowel changes
Most people have an ileostomy after surgery. People who do not have an ileostomy may have diarrhea (loose or watery bowel movements) while they’re in the hospital. Your care team will help you manage it.
Showering
Wash your face, brush your teeth, and change your pajamas every day. Ask one of your healthcare providers for help if you need it.
You’ll be able to shower with help 48 hours (2 days) after your last tube or drain is removed.
Getting chemo
If you’re getting chemo as part of your cancer treatment, you may have a chemo treatment while you’re in the hospital. Your care team will talk with you about what to expect.
If your care team closer to home manages your chemo, your MSK care team will work with them to plan and manage your treatment.
Leaving the hospital
By the time you’re ready to leave the hospital, your incision will have started to heal. Before you leave, look at your incision with your caregiver and one of your healthcare providers. Knowing what it looks like will help you notice any changes later.
Before you’re discharged, your healthcare provider will write your discharge order and prescriptions. You’ll also get written discharge instructions. One of your healthcare providers will review these instructions with you before you leave.
At home
Filling out your Recovery Tracker
We want to know how you’re feeling after you leave the hospital. To help us care for you, we’ll send questions to your MSK MyChart account. We’ll send them every day for 10 days after you’re discharged. These questions are known as your Recovery Tracker.
Fill out your Recovery Tracker every day before midnight (12 a.m.). It only takes 2 to 3 minutes to complete. Your answers to these questions will help us understand how you’re feeling and what you need.
Based on your answers, we may reach out to you for more information. Sometimes, we may ask you to call your surgeon’s office. You can always contact your surgeon’s office if you have any questions.
To learn more, read Common Questions About MSK's Recovery Tracker.
Managing your pain
People have pain or discomfort for different lengths of time. You may still have some pain when you go home and will probably be taking pain medicine. Some people have soreness, tightness, or muscle aches around their incision for a month or two. This doesn’t mean something is wrong.
Follow these guidelines to help manage your pain at home.
- Take your medicines as directed and as needed.
- Call your healthcare provider if the medicine prescribed for you does not help your pain.
- Do not drive or drink alcohol while you’re taking prescription pain medicine. Some prescription pain medicines can make you drowsy (very sleepy). Alcohol can make the drowsiness worse.
-
You’ll have less pain and need less pain medicine as your incision heals. An over-the-counter pain reliever will help with aches and discomfort. Acetaminophen (Tylenol®) and ibuprofen (Advil or Motrin) are examples of over-the-counter pain relievers.
- Follow your healthcare provider’s instructions for stopping your prescription pain medicine.
- Do not take too much of any medicine. Follow the instructions on the label or from your healthcare provider.
- Read the labels on all the medicines you’re taking. This is very important if you’re taking acetaminophen. Acetaminophen is an ingredient in many over-the-counter and prescription medicines. Taking too much can harm your liver. Do not take more than one medicine that has acetaminophen without talking with a member of your care team.
- Pain medicine should help you get back to your usual activities. Take enough to do your activities and exercises comfortably. You may have a little more pain as you start to be more active.
- Keep track of when you take your pain medicine. It works best 30 to 45 minutes after you take it. Taking it when you first have pain is better than waiting for the pain to get worse.
Some prescription pain medicines, such as opioids, may cause constipation. Constipation is when you poop less often than usual, have a harder time pooping, or both.
Preventing and managing constipation
Talk with your healthcare provider about how to prevent and manage constipation. You can also follow these guidelines.
- Be physically active, if you can.
-
Talk with your clinical dietitian nutritionist about how much liquid you should drink each day. Aim to drink that much every day.
- Choose liquids such as water, juices (such as prune, grape, or pear juice), soups, and ice cream shakes.
- Avoid liquids with caffeine (such as coffee and soda). Caffeine can pull fluid out of your body.
- Both over-the-counter and prescription medicines can treat constipation. Check with your healthcare provider before taking any medicines for constipation,. especially That’s very important if you have an ileostomy or have had bowel surgery.
Caring for your incision
If your drain was removed just before you were discharged from the hospital, you may have a dressing (bandage) over the area. You can take it off after 24 to 48 hours (1 to 2 days). Follow your healthcare provider’s instructions.
Call your healthcare provider’s office if:
- The skin around your incision is very red.
- The skin around your incision is getting more red.
- You see drainage that looks like pus (thick and milky).
- Your incision smells bad.
Showering or bathing
You can follow your usual shower routine, unless you were discharged with a drain. If you have a drain, do not shower until your care team takes it out.
Do not put your incision underwater (such as in a bathtub or pool) for 14 days after your surgery.
Eating and drinking
An MSK Kids clinical dietitian nutritionist will help you manage your diet and nutrition after you’re discharged from the hospital. They’ll talk with you about foods in your diet to help you heal after surgery, gain weight, or both. You can also read Diet Guidelines for People With an Ileostomy to learn more.
If you’re getting tube feeds at home, your MSK Kids clinical dietitian nutritionist will talk with you about your tube feeding schedule and rate.
Call your healthcare provider if your appetite isn’t back to normal after a few days or if you start vomiting (throwing up).
Preventing dehydration
It’s very important to drink lots of liquids while you have a temporary ileostomy. You can get dehydrated if you’re eating and drinking less than the amount of poop your body is making.
Drink 8 to 10 (8-ounce) cups of liquids every day. Call your healthcare provider if you have any of these signs or symptoms of dehydration:
- You feel thirstier than normal.
- Your mouth is dry.
- Your skin is dry.
- You have fatigue (feel more tired than normal).
- You have appetite loss.
- You feel dizzy when you stand.
- You have a headache.
- You have leg cramps.
Signs of a bowel obstruction
There’s a higher chance you will get a bowel obstruction while you have a temporary ileostomy. A bowel obstruction is when your intestine is blocked partly or all the way blocked. This keeps food, liquids, and gas from moving through your intestines like normal. Food, scar tissue, or a twist in your intestine can cause a bowel obstruction.
Call your healthcare provider if you have any of these signs or symptoms of a bowel obstruction:
- Your belly is tender and bloated (swollen).
- You have belly cramps.
- You have nausea or vomiting.
- You cannot pass gas or stool.
- There’s less or no output from your ileostomy.
Physical activity and exercise
You can go back to doing most of your usual activities once you’re home. Avoid contact sports and roughhousing for about 6 weeks after surgery. It takes about that long for your incision to heal.
If you have questions about living with an ileostomy, talk with your WOC nurse.
Going back to school or work
You can go back to school or work as soon as you feel ready.
Traveling
Most people do not need to follow any special guidelines for traveling. It’s OK to travel on a plane.
Follow-up appointment
Your surgeon’s office may schedule your follow-up appointment before you’re discharged from the hospital. Or, they may call you to schedule it once you’re home. Your follow-up appointment can be done either in-person or by telemedicine.
When to call your healthcare provider
Call your healthcare provider if:
- Your incision is starting to look red.
- Redness around your incision is getting worse.
- There’s liquid draining from your incision.
- The area around your incision is starting to swell.
- Swelling around your incision is getting worse.
- You have appetite loss (don’t feel a desire to eat).
- You’re vomiting (throwing up).
- You have an ileostomy and have not had a bowel movement for 3 to 6 hours.
-
You start to have abdominal pain or symptoms of dehydration, including:
- Increased thirst
- Dry mouth
- Loss of appetite
- Weakness
- Lower urine output
- Dark, amber-colored urine
- Muscle, abdominal, or leg cramps
- Feeling faint
- More bowel movements than usual or changes in your bowel movements’ consistency
- Emptying your pouch more often than usual
- Your stoma looks dark red, grey, brown, or black. Call your healthcare provider right away.
- You notice blood in your bowel movements or coming from inside your stoma. Call your healthcare provider right away.
- You have any questions or concerns.
Contact information
If you have questions or concerns, contact your healthcare provider. A member of your care team will answer Monday through Friday from to Outside those hours, you can leave a message or talk with another MSK provider. There is always a doctor or nurse on call.
If you’re not sure how to reach your healthcare provider, call 212-639-2000.
Support services
This section has a list of support services. They may help you as you get ready for your surgery and recover after your surgery.
As you read this section, write down questions to ask your healthcare provider.
MSK support services
Admitting Office
212-639-7606
Call if you have questions about your hospital admission, such as asking for a private room.
Anesthesia
212-639-6840
Call if you have questions about anesthesia.
Blood Donor Room
212-639-7643
Call for information if you’re interested in donating blood or platelets.
Bobst International Center
www.msk.org/international
888-675-7722
We welcome patients from around the world and offer many services to help. If you’re an international patient, call for help arranging your care.
Counseling Center
www.msk.org/counseling
646-888-0200
Many people find that counseling helps them. Our Counseling Center offers counseling for individuals, couples, families, and groups. We can also prescribe medicine to help if you feel anxious or depressed. Ask a member of your care team for a referral or call the number above to make an appointment.
Food Pantry Program
646-888-8055
We give food to people in need during their cancer treatment. Talk with a member of your care team or call the number above to learn more.
Integrative Medicine and Wellness Service
www.msk.org/integrativemedicine
Our Integrative Medicine and Wellness Service offers many services to complement (go along with) traditional medical care. For example, we offer music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. Call 646-449-1010 to make an appointment for these services.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine and Wellness Service. They’ll work with you to make a plan for creating a healthy lifestyle and managing side effects. Call 646-608-8550 to make an appointment for a consultation.
MSK Library
library.mskcc.org
You can visit our library website or email [email protected] to talk with the library reference staff. They can help you find more information about a type of cancer. You can also visit the library’s Patient Education Resource Guide.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian nutritionists. Your clinical dietitian nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. Ask a member of your care team for a referral or call the number above to make an appointment.
Patient and Community Education
www.msk.org/pe
Visit our patient and community education website to search for educational resources, videos, and online programs.
Patient Billing
646-227-3378
Call if you have questions about preauthorization with your insurance company. This is also called preapproval.
Patient Representative Office
212-639-7202
Call if you have questions about the Health Care Proxy form or concerns about your care.
Perioperative Nurse Liaison
212-639-5935
Call if you have questions about MSK releasing any information while you’re having surgery.
Private Duty Nurses and Companions
646-357-9272
You can request private nurses or companions to care for you in the hospital and at home. Call to learn more.
Rehabilitation Services
www.msk.org/rehabilitation
Cancers and cancer treatments can make your body feel weak, stiff, or tight. Some can cause lymphedema (swelling). Our physiatrists (rehabilitation medicine doctors), occupational therapists (OTs), and physical therapists (PTs) can help you get back to your usual activities.
- Rehabilitation medicine doctors diagnose and treat problems that affect how you move and do activities. They can design and help coordinate your rehabilitation therapy program, either at MSK or somewhere closer to home. Call Rehabilitation Medicine (Physiatry) at 646-888-1929 to learn more.
- An OT can help if you’re having trouble doing usual daily activities. For example, they can recommend tools to help make daily tasks easier. A PT can teach you exercises to help build strength and flexibility. Call Rehabilitation Therapy at 646-888-1900 to learn more.
Resources for Life After Cancer (RLAC) Program
646-888-8106
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
Sexual Health Programs
Cancer and cancer treatments can affect your sexual health, fertility, or both. MSK’s sexual health programs can help you before, during, or after your treatment.
- Our Female Sexual Medicine and Women’s Health Program can help with sexual health problems such as premature menopause or fertility issues. Ask a member of your MSK care team for a referral or call 646-888-5076 to learn more.
- Our Male Sexual and Reproductive Medicine Program can help with sexual health problems such as erectile dysfunction (ED). Ask a member of your care team for a referral or call 646-888-6024 to learn more.
Social Work
www.msk.org/socialwork
212-639-7020
Social workers help patients, families, and friends deal with common issues for people who have cancer. They provide individual counseling and support groups throughout your treatment. They can help you communicate with children and other family members.
Our social workers can also help refer you to community agencies and programs. If you’re having trouble paying your bills, they also have information about financial resources. Call the number above to learn more.
Spiritual Care
212-639-5982
Our chaplains (spiritual counselors) are available to listen, help support family members, and pray. They can contact community clergy or faith groups, or simply be a comforting companion and a spiritual presence. Anyone can ask for spiritual support. You do not have to have a religious affiliation (connection to a religion).
MSK’s interfaith chapel is located near Memorial Hospital’s main lobby. It’s open 24 hours a day. If you have an emergency, call 212-639-2000. Ask for the chaplain on call.
Tobacco Treatment Program
www.msk.org/tobacco
212-610-0507
If you want to quit smoking, MSK has specialists who can help. Call to learn more.
Virtual Programs
www.msk.org/vp
We offer online education and support for patients and caregivers. These are live sessions where you can talk or just listen. You can learn about your diagnosis, what to expect during treatment, and how to prepare for your cancer care.
Sessions are private, free, and led by experts. Visit our website to learn more about Virtual Programs or to register.
External support services
Access-A-Ride
web.mta.info/nyct/paratran/guide.htm
877-337-2017
In New York City, the MTA offers a shared ride, door-to-door service for people with disabilities who can’t take the public bus or subway.
Air Charity Network
www.aircharitynetwork.org
877-621-7177
Provides travel to treatment centers.
American Cancer Society (ACS)
www.cancer.org
800-ACS-2345 (800-227-2345)
Offers a variety of information and services, including Hope Lodge, a free place for patients and caregivers to stay during cancer treatment.
Cancer and Careers
www.cancerandcareers.org
646-929-8032
A resource for education, tools, and events for employees with cancer.
CancerCare
www.cancercare.org
800-813-4673
275 Seventh Avenue (Between West 25th & 26th Streets)
New York, NY 10001
Provides counseling, support groups, educational workshops, publications, and financial assistance.
Cancer Support Community
www.cancersupportcommunity.org
Provides support and education to people affected by cancer.
Caregiver Action Network
www.caregiveraction.org
800-896-3650
Provides education and support for people who care for loved ones with a chronic illness or disability.
Corporate Angel Network
www.corpangelnetwork.org
866-328-1313
Offers free travel to treatment across the country using empty seats on corporate jets.
Good Days
www.mygooddays.org
877-968-7233
Offers financial assistance to pay for copayments during treatment. Patients must have medical insurance, meet the income criteria, and be prescribed medicine that’s part of the Good Days formulary.
HealthWell Foundation
www.healthwellfoundation.org
800-675-8416
Provides financial assistance to cover copayments, health care premiums, and deductibles for certain medicines and therapies.
Joe’s House
www.joeshouse.org
877-563-7468
Provides a list of places to stay near treatment centers for people with cancer and their families.
LGBT Cancer Project
www.lgbtcancer.com
Provides support and advocacy for the LGBT community, including online support groups and a database of LGBT-friendly clinical trials.
LIVESTRONG Fertility
www.livestrong.org/fertility
855-744-7777
Provides reproductive information and support to cancer patients and survivors whose medical treatments have risks associated with infertility.
Look Good Feel Better Program
www.lookgoodfeelbetter.org
800-395-LOOK (800-395-5665)
This program offers workshops to learn things you can do to help you feel better about your appearance. For more information or to sign up for a workshop, call the number above or visit the program’s website.
National Cancer Institute
www.cancer.gov
800-4-CANCER (800-422-6237)
National Council on Aging (NCOA)
www.benefitscheckup.org
Provides information and resources for older adults. Offers BenefitsCheckUp®, a free online tool that connects you to prescription assistance programs, including Medicare’s Extra Help program.
National LGBT Cancer Network
www.cancer-network.org
Provides education, training, and advocacy for LGBT cancer survivors and those at risk.
Needy Meds
www.needymeds.org
Lists Patient Assistance Programs for brand and generic name medicines.
NYRx
www.health.ny.gov/health_care/medicaid/program/pharmacy.htm
Provides prescription benefits to eligible employees and retirees of public sector employers in New York State.
Patient Access Network (PAN) Foundation
www.panfoundation.org
866-316-7263
Gives help with copayments for patients with insurance.
Patient Advocate Foundation
www.patientadvocate.org
800-532-5274
Provides access to care, financial assistance, insurance assistance, job retention assistance, and access to the national underinsured resource directory.
Red Door Community (formerly known as Gilda’s Club)
www.reddoorcommunity.org
212-647-9700
A place where people living with cancer find social and emotional support through networking, workshops, lectures, and social activities.
RxHope
www.rxhope.com
877-267-0517
Provides assistance to help people get medicines they have trouble affording.
Triage Cancer
www.triagecancer.org
Provides legal, medical, and financial information and resources for cancer patients and their caregivers.
Educational resources
This section lists the educational resources mentioned in this guide. They will help you get ready for your surgery and recover after your surgery.
As you read these resources, write down questions to ask your healthcare provider.
- A Guide for Caregivers
- Common Questions About MSK's Recovery Tracker
- Advance Care Planning for People With Cancer and Their Loved Ones
- Caring for Your Ileostomy or Colostomy
- Diet Guidelines for People With an Ileostomy
- Frequently Asked Questions About the Goals to Discharge Checklist
- Frequently Asked Questions About Walking After Your Surgery
- Herbal Remedies and Cancer Treatment
- How to Be a Health Care Agent
- How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil
- How To Do Bowel Prep Before Your Surgery at MSK Kids
- How To Use Your Incentive Spirometer
- Information for Family and Friends for the Day of Surgery
- Liquid Intake and Ostomy Output Log
- Patient-Controlled Analgesia (PCA)
- Staying Active Before and After Surgery for Pediatric Patients


