This information explains what T1DM is and how to manage it. It also explains how immunotherapy or having your pancreas removed can cause T1DM. It also has information about the basic skills and important safety measures you’ll need to safely manage T1DM.
About diabetes
Diabetes is a lifelong health condition that affects how the body processes blood sugar (glucose). Glucose is a main source of energy for cells and comes from the foods we eat. Special cells in the pancreas produce the hormone insulin. Insulin helps the body manage and use glucose effectively.
In diabetes, the body either does not produce enough insulin or cannot use insulin effectively. In some cases, the body completely stops making insulin. This leads to high blood glucose levels. Over time, this can cause damage to the organs and tissues in the body.
Diabetes affects nearly every part of the body and can lead to serious health complications if not managed well. Taking insulin and making lifestyle changes will help you manage T1DM and keep your blood sugar at safe levels.
Common questions about diabetes
I have a lot going on with my cancer treatment and feel like I cannot handle it all. Is it OK to wait to start managing type 1 diabetes?
It’s normal to feel overwhelmed during cancer treatment, but your body needs insulin to survive. It’s important to manage T1DM right away. Waiting to treat T1DM can lead to serious health problems that can be fatal. Serious illness can also interfere with your cancer care.
You care team will support you and work with you to make a plan that fits into your treatment schedule.
How can I prevent other health issues caused by diabetes?
There is no cure for diabetes. Keeping your body at a healthy weight can help it use insulin more easily. It also helps your body manage your blood glucose levels.
Controlling your blood glucose levels is the best way to prevent other health issues caused by diabetes. You can do this by taking your insulin as prescribed.
Knowing your blood glucose level is the first step to preventing hyperglycemia. Check your blood glucose regularly. Read About Hyperglycemia (High Blood Sugar) to learn more.
Keep a healthy lifestyle through diet and exercise. To learn more about eating a healthy diet, call 212-639-7312 to talk with a clinical dietitian-nutritionist.
About Newly Diagnosed Type 1 Diabetes Mellitus (T1DM)
This information explains what type 1 diabetes mellitus (T1DM) is and what causes it. It also explains how to manage T1DM after you get diagnosed.
About type 1 diabetes mellitus
Type 1 diabetes mellitus (dy-uh-BEE-teez MEH-lih-tus) is also called T1DM. It’s an autoimmune disease, which means your body attacks its own healthy tissues and organs.
T1DM is when your body kills the cells in the pancreas that make insulin. Your body can no longer make insulin on its own. Insulin is a hormone that helps glucose (sugar) enter cells and provide energy. Without insulin, your blood glucose level can become very high, enough to harm you. This is called hyperglycemia (HY-per-gly-SEE-mee-uh), also known as high blood sugar.
Autoimmune T1DM often starts in childhood, but it can happen at any age.
T1DM is permanent (does not go away). You’ll need to treat it all of your life. People with T1DM must take insulin injections (shots) to replace the insulin their body cannot make. Read About Insulin for Diabetes or Treatment-Related Hyperglycemia to learn more.
Treatments that can cause T1DM
Immunotherapy
Immunotherapy is a treatment that boosts your immune system to help fight diseases like cancer. Some immunotherapies can also target the cells that make insulin in your pancreas while fighting the cancer cells.
T1DM is a rare but serious side effect of these treatments. About 1 in 100 people who get immunotherapy develop T1DM.
Total pancreatectomy
A total pancreatectomy (PAN-kree-uh-TEK-toh-mee) is a surgery to take out all of your pancreas. This is sometimes done to treat problems that are precancerous (can become cancer).
The pancreas is the only organ that makes insulin, and people who have this surgery can no longer make insulin. This causes T1DM.
How to manage T1DM
Diabetes can cause long-term health problems. It’s important to manage diabetes during cancer treatment.
If you are newly diagnosed with T1DM, it’s very important to learn how to stay safe and healthy. Here are some tips and reminders to keep you safe.
Test your blood glucose
Your goal is to keep your blood glucose (BG) level between 100 and 200 milligrams/deciliter (mg/dL). You’ll use a glucometer or a continuous glucose monitor (CGM) to test your glucose.
Most people test their glucose when they wake up, before meals, and at bedtime. This will help you decide how to manage your blood glucose.
- Have your supplies with you. Even if you’re using a CGM, always have your blood glucose meter and testing supplies with you as a backup. These include a lancing device, test strips, and lancets. Doing a fingerstick can help you make sure your CGM glucose reading is correct. This lets you decide how to manage your glucose. Read About Your Continuous Glucose Monitor (CGM) to learn more.
- Check your blood glucose often. Avoid going for more than 6 hours without checking your blood glucose, unless you’re asleep.
- Keep track of your supplies. Be sure to regularly keep track of how much you have so you do not run out. You may be able to get these supplies at a lower cost with a prescription. Talk to your diabetes healthcare provider about getting a prescription for these supplies. You can also buy blood glucose testing strips over the counter if you run out.
Use insulin safely
People with T1DM must take both rapid-acting and long-acting insulin. Rapid-acting means it starts to work right away. Rapid-acting insulin helps manage the rise in blood glucose that happens after eating. Long-acting means it works for a longer time. Long-acting insulin helps manage your blood glucose between meals and while you sleep.
Follow your diabetes healthcare provider’s instructions for taking insulin. Read About Your Continuous Glucose Monitor (CGM) About Insulin for Diabetes or Treatment-Related Hyperglycemia to learn more.
Always have at least 1 extra of each insulin pen. Keep these in the refrigerator until you use them. Read How to Use an Insulin Pen to learn more.
Rapid-acting insulin
Most people take rapid-acting insulin a few times a day, before each meal. Rapid-acting insulin works for 4 hours. Take rapid-acting insulin within 15 minutes before your meal, at least 4 hours apart.
Your diabetes provider may tell you to take a correctional dose of insulin whether you are eating or not. If they do, follow their instructions. A correctional dose is an extra dose of rapid-acting insulin. This helps to lower your blood glucose and manage hyperglycemia.
When taking rapid-acting insulin, try not to miss any meals. If you do, you should still check your blood glucose. To help prevent hypoglycemia (low blood sugar), only take mealtime rapid-acting insulin if you’re eating at least 30 grams of carbohydrates. Read How To Manage Your Blood Glucose (Blood Sugar) With Your Diet to learn more.
Long-acting insulin
Long-acting insulin helps keep your blood glucose levels stable when you’re not eating. Examples are between meals and throughout the night. Most people take long-acting insulin once or twice a day.
If you take long-acting insulin once a day, take the dose at the same time every day.
If you take long-acting insulin twice a day, take the doses 12 hours apart at the same time every day.
Manage hyperglycemia
Hyperglycemia is when your blood glucose level goes above 200 mg/dL. This can happen if you eat too many carbohydrates or do not take enough insulin.
Symptoms of hyperglycemia include feeling like you need to urinate (pee) often, feeling very thirsty, and having dry mouth. Read About Hyperglycemia (High Blood Sugar) to learn more.
If you eat a snack between meals, do not take extra insulin. Taking insulin doses too close together can cause hypoglycemia.
To prevent hyperglycemia, limit the amount of carbohydrates in your snack. Instead, eat something high in protein or non-starchy vegetables. High protein snacks include a serving of cheese, peanut butter, or Greek yogurt. Non-starchy vegetables include spinach, mushrooms, broccoli, and peppers.
Prevent diabetic ketoacidosis (DKA)
Diabetes ketoacidosis (DKA) is a medical emergency that happens when your body does not have enough insulin. DKA can be life-threatening (it can cause death). If you have DKA or think you have DKA, call for medical help right away. Read Diabetic Ketoacidosis (DKA) and Ketone Urine Testing to learn more.
Symptoms of DKA include:
- Urinating (peeing) often.
- Extreme thirst (feeling thirsty even after drinking a lot of fluids).
- Fruity-smelling breath.
- Deep, fast breathing.
- Feeling confused.
- Abdominal (belly) pain.
To prevent DKA:
- Never skip your long-acting insulin dose. If your blood glucose is low and you are concerned, call your diabetes provider. They’ll give you instructions or talk with you about the best plan for you.
- Be ready to manage your diabetes when you have “sick days.” Never stop taking your insulin before you talk with your diabetes healthcare provider first. Read How to Manage Diabetes When You’re Sick to learn more.
Treat hypoglycemia (low blood sugar)
Hypoglycemia is when your blood glucose level goes below 70 mg/dL. This can happen if you did not eat enough or are more active than usual. Symptoms of hypoglycemia include shakiness, fast heartbeats, dizziness, and sweating. Read About Hypoglycemia (Low Blood Sugar) to learn more.
It’s important to treat hypoglycemia right away. Always carry something with you that has 15 grams (g) of rapid-acting sugar to treat hypoglycemia. This includes glucose tablets or 4 ounces of juice. Contact the provider who prescribes your diabetes medicine any time you have hypoglycemia.
If you had a total pancreatectomy, you may not always have the symptoms of hypoglycemia. Try to have the same amount of carbohydrates with every meal as much as possible. This will help balance your blood glucose level. It will also help your diabetes healthcare provider know how much insulin you need.
Prevent hypoglycemia
It’s best to prevent hypoglycemia before your blood glucose goes below 70 mg/dL. When your blood glucose is between 70 and 99 mg/dL, it’s important to have a balanced snack. Your snack should include:
- Something high in protein, such as a serving of cheese, peanut butter, or Greek yogurt.
- One serving of a carbohydrate, such as a small apple, half a banana, a slice of toast, or 6 small crackers. A serving of carbohydrates is equal to 15 grams.
Avoid having a rapid-acting sugar, such as juice or soda. This can cause your blood glucose to go too high. Read How To Manage Your Blood Glucose (Blood Sugar) With Your Diet to learn more.
Hypoglycemia unawareness
Your body gives you warning signs when your blood sugar drops too low. These include feeling shaky, sweaty, hungry, dizzy, or anxious. These warning signs tell you something is wrong so you can treat the low blood sugar right away.
Hypoglycemia unawareness is when your body stops giving you those warning signs. Your blood sugar can drop to a harmful level without you knowing. This is common in people who have had diabetes for many years. It’s also common if you have low blood glucose very often.
Over time, your body gets used to hypoglycemia and stops reacting the way it should. You may pass out without showing any other signs or symptoms.
It can be very harmful and lead to a medical emergency if you do not get treated right away. This is why it’s important to check your blood glucose regularly. Follow your diabetes healthcare provider’s instructions for how often you should check your blood glucose.
Things to buy if you have T1DM
These things can help you manage T1DM:
- Ketone test strips. Use these to measure the ketones in your urine.
-
Medical alert bracelet. This will help first responders provide the right care if you have a medical emergency. The bracelet should say either:
- T1DM
- Type 1DM
- Type 1 diabetes
- Glucose tablets or glucose gel. These are easy to carry with you when you’re not home.
- A food scale. This can help you measure portion sizes and learn how much food is in a serving.
You can buy these things online or at your local drugstore. You do not need a prescription.
How to Check Your Blood Sugar Using a Blood Glucose Meter
This information describes how to check your blood glucose level using a blood glucose meter.
The steps in this resource are specific to the Contour® Next One blood glucose meter and Microlet® Next lancing device. If you’re using a different type of blood glucose meter or lancing device, follow the instructions that came with it. All blood glucose meters and lancing devices are slightly different.
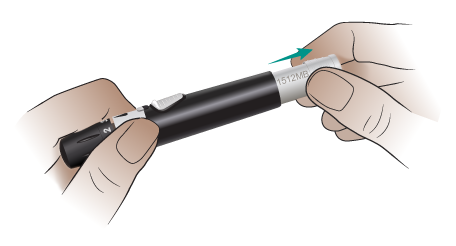
About the Microlet Next lancing device
Your lancing device holds the lancet (needle) you’ll use to prick your finger. It has 6 main parts (see Figure 1).
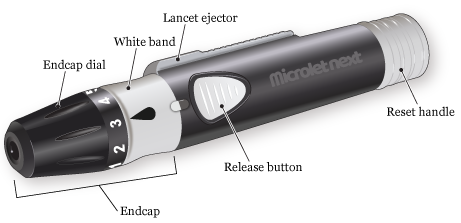
- The endcap covers the lancet until you’re ready to use it.
- The endcap dial controls how deeply the lancet will prick your finger.
- The white band connects the endcap to the rest of the lancing device. The endcap is locked onto the lancing device when the black drop is in line with the release button.
- The release button makes the tip of the lancet spring out to prick your finger.
- The reset handle resets the lancet if you need to prick your finger again.
- The lancet ejector pushes the lancet out of the lancing device once you’re done using it.
Your Microlet Next lancing device works with Microlet lancets. Microlet Next lancets come in different colors, but there’s no difference between them.
About your Contour Next One blood glucose meter
A blood glucose meter measures the amount of sugar in your blood. It has 3 main parts (see Figure 2).
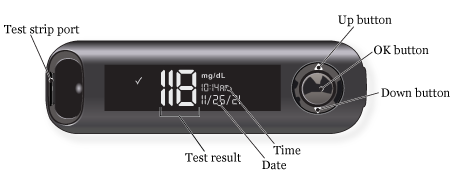
- The test strip port is where you’ll put the blood glucose test strip into the meter. Your Contour Next One glucose meter will only work with Contour Next test strips.
- The screen shows information such as the meter’s status, your blood glucose level, and the date and time.
-
The buttons are how you control the meter.
- To scroll up, press the up button. Hold it to keep scrolling.
- To scroll down, press the down button. Hold it to keep scrolling.
- To accept a selection, press the OK button.
- To turn your meter on or off, press and hold the OK button.
You need to set up your meter before using it for the first time.
You do this by:
- Accepting the blood glucose target range of 70-180 milligrams per deciliter (mg/dL).
- Setting the time.
- Setting the date.
Your meter will not work until you set it up.
Watch Contour® Next One Video: Doing Your First Test for instructions on how to set up your meter.
Do not put your glucose meter under water. If you notice it’s dirty, wipe it with a damp cloth or alcohol pad.
The Contour Diabetes app
The Contour Diabetes app works with your Contour Next One blood glucose meter. It lets you make notes, set reminders, see your results in a graph, and share your reports. If you want to use the app, you can download it from the Apple App Store® or Google Play™ store.
You do not need to download the Contour Diabetes app if you do not want to. The Contour Next One blood glucose meter works without the app.
The Contour Next One user guide
To learn more about the Contour Next One blood glucose meter and Contour Diabetes app, read the Contour Next One user guide. You can read the copy that came with your meter or find it at www.contournextone.com/getting-started.
Instructions for checking your blood sugar
Your healthcare provider will tell you how often to check your blood glucose. They’ll also tell you what your blood glucose level should be. This is called your blood glucose target range. Your blood glucose target range is based on your overall health and current treatment plan.
When you’re ready to start, wash your hands with soap and water. Dry them very well. Touching a blood glucose test strip with damp hands can damage it or make your result less accurate.
Gather your supplies
Set up your supplies on a clean surface. It’s helpful to arrange them in the order you’ll use them (see Figure 3).

You’ll need:
- Your lancing device.
- A new lancet.
- Your blood glucose meter.
- Your blood glucose test strips.
- An alcohol pad (if you do not have access to a sink to wash your hands).
- A dry tissue or gauze pad (if you do not have access to a sink to wash your hands).
- Your blood glucose log.
- A trash can.
- A solid container to throw away the used lancet, such as a heavy plastic laundry detergent bottle with a lid. Read How to Store and Get Rid of Your Home Medical Sharps for more information about choosing a container.
When you take a blood glucose test strip out of the container, set it on top of your meter. This helps keep it clean and dry and makes it easier to pick up. Make sure to close the glucose test strip container tightly. Humidity from the air can damage the strips.
Get your lancing device ready
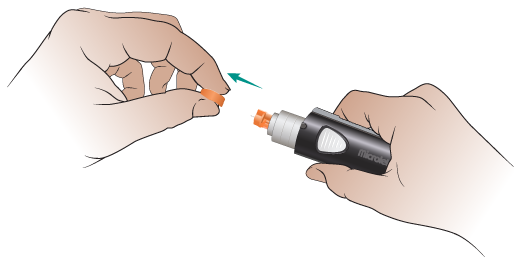
-
Twist the white band on your lancing device to the right to unlock the endcap (see Figure 4).
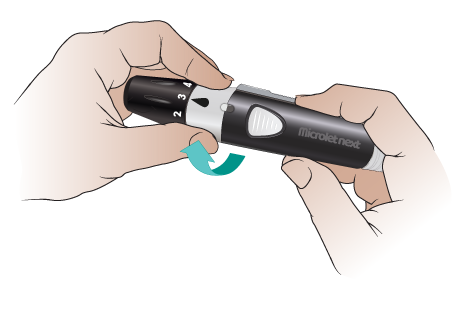
Figure 4. Twist the white band to the right - Pull the endcap straight off (see Figure 5).
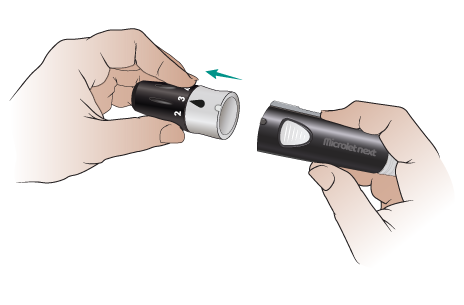
- Carefully twist the round tab 3 times. Be careful not to bend it. Pull the tab off and set it aside to use later (see Figure 6). You should see a small needle where the tab was.
- Put the endcap back on your lancing device in the unlocked position (see Figure 7).
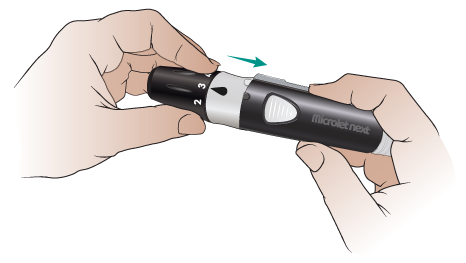
-
Twist the white band to the left to lock the endcap on (see Figure 8).
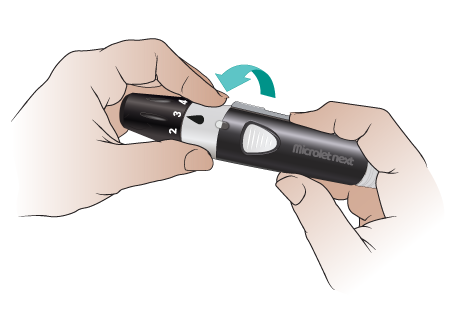
Figure 8. Twist the white band to the left -
Turn the black part of the endcap dial to set the puncture depth (see Figure 9). It’s best to start with level 1 or 2. You can set it to a higher level if you do not get a big enough blood drop.

Figure 9. Set the puncture depth
Your lancing device is now ready. Set it down. Pick up your blood glucose meter and test strip.
Get your blood glucose meter ready
- Hold the test strip with the printed side facing you.
- Hold your blood glucose meter with the screen and buttons facing you.
-
Put the grey square end of the test strip into your meter’s test strip port (see Figure 10).

Figure 10. Put the test strip into the port
Your meter should beep and turn on after you put the test strip in the port. If it does not:
- Make sure you pushed the test strip all the way into the port.
- Make sure the end of the test strip with the grey square is in the port.
- Make sure the printed side of the test strip is facing you.
Your blood glucose meter is now ready. It will stay on for 3 minutes after you put in the test strip. If you do not apply a drop of blood to the tip of the test strip in that time, it will beep and turn off. If this happens, pull the test strip out and put it back into the port.
Do not apply blood to the test strip before you put it into the meter or when the meter is off. If you do, that strip will be ruined. You’ll have to start over with a new one.
Prick your finger
-
Choose which finger you’re going to prick. We recommend using the side of your fingertip (see Figure 11). The middle and top of your fingertip are more sensitive.
- Use a different spot each time. This will help prevent sore spots. Remember that you can use both sides of each fingertip.
- If you have not already washed your hands, clean the area with the alcohol pad. Dry it with the clean tissue or gauze pad.
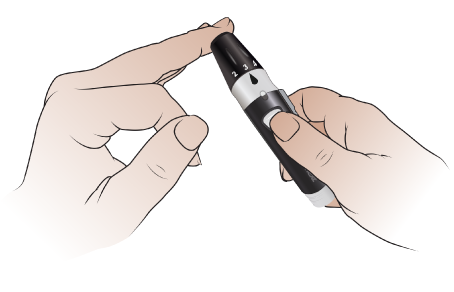
Figure 11. Hold the lancing device firmly against the side of your finger -
Hold your lancing device firmly against the side of your finger (see Figure 12) and press the release button. Then move the lancing device away from your finger right away. Look for a blood drop.You may need to gently massage or squeeze your finger (see Figure 12). Do not do this too hard. If you do, your results may not be accurate.If the blood drop is too small, you’ll need to prick your finger again. It’s OK to use the same lancet.

Figure 12. Gently squeeze your finger to get a blood drop
a. Pull the white reset handle on your lancing device until you hear it click into place (see Figure 13).
b. Turn the endcap dial to increase the puncture depth by 1 level.
c. Make sure you have the lancing device pressed firmly against the side of your finger.
d. Press the release button. Then move your lancing device away from your finger right away.
e. Look for a blood drop. You may need to massage your finger gently. If the blood drop is bigger than you needed, lower the puncture depth by 1 next time you use your lancing device. This means the lancet will not prick your finger as deeply.
Touch the blood glucose test strip to the blood drop
-
Once you have a big enough blood drop, touch the tip of the test strip to the drop (see Figure 14). The blood will be drawn into the test strip. Putting the blood on the top, bottom, or side of the strip will not work.
- If there is not enough blood on the first try, your meter will beep twice, and a blood drop will flash on the display. You can apply more blood to the test strip within 60 seconds.
- If you do not apply enough blood within 60 seconds, your meter will show an error code. If this happens, pull out the test strip and throw it away. Start again with a new test strip. Increase the puncture depth on your lancing device, if needed.
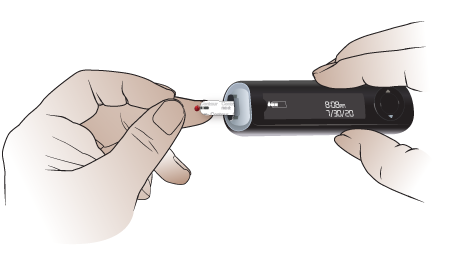
Figure 14. Touch the end of the test strip -
When you’ve applied enough blood to the test strip, your meter will beep and count down from 5. Your blood glucose level will appear on the screen and you’ll see a color near the test strip port. This is called the Target Light or smartLIGHT. You’ll see green if your result is in the target range, yellow if it’s too high, or red if it’s too low.
- When you first get your Contour Next One blood glucose meter, the target blood glucose range will be 70 to 180 mg/dL.
- If your diabetes provider gives you a different target range, you can change it using the Contour Diabetes app.
- If you do not want to use the smartLIGHT feature, you can turn it off using the Contour Diabetes app.
Write down your blood sugar level
Write your blood glucose level in your blood glucose log. Your result will stay on the screen until you take out the test strip or for 3 minutes.
Make sure your blood glucose meter is right-side up when you read it. To quickly check, make sure you can read the time and date.
Throw away the test strip and used lancet
-
Firmly pull the test strip out of your blood glucose meter (see Figure 15). Throw it away in the trash can. It’s OK to put it with your regular trash.

Figure 15. Pull the test strip out of your blood glucose meter - Twist the white band on your lancing device to the right to unlock the endcap. Pull the endcap straight off.
-
Put the round plastic tab you removed from the top of the lancet earlier on a flat surface. Push the end of the lancet firmly into the plastic tab (see Figure 16). The tab will cover the lancet so you will not accidentally prick yourself.
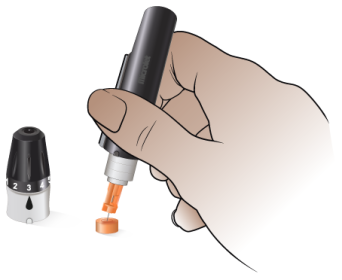
Figure 16. Push the end of the lancet into the plastic tab -
Hold the lancet over your plastic sharps container. Slide the lancet ejector forward until the lancet falls into the plastic sharps container (see Figure 17).
- Do not pull the lancet out with your fingers. The plastic tab can easily come off. If it does, you may prick yourself with the needle.

Figure 17. Eject the lancet into the sharps container - Slide the lancet ejector back into place. Put the endcap back on your lancing device. Twist the white band to the left to lock on the endcap.
Keeping track of your results
- Your healthcare provider will tell you how to keep track of your blood glucose levels and medicine doses. Follow their instructions.
- Bring your blood glucose log to all your appointments. This information will help your healthcare provider decide if they should change your current treatment plan. If you have questions about checking your blood glucose, ask your healthcare provider.
Where to buy supplies
Talk with your diabetes healthcare provider to get a refill prescription for blood glucose test strips and lancets. You must get refills from your local pharmacy. MSK’s outpatient pharmacy does not carry these supplies.
If your blood glucose meter is battery-powered, make sure to always have extra batteries. The Contour Next One blood glucose meter uses 2 CR-2032 batteries. You can buy these batteries online or at your local electronics store, hardware store, or supermarket.
Contour Next One Video - Doing your first test
About Hyperglycemia (High Blood Sugar)
This information describes hyperglycemia (HY-per-gly-SEE-mee-uh), what causes it, and how to recognize, prevent and treat it. It also talks about different types of diabetes.
What is hyperglycemia?
Hyperglycemia is when too much glucose (sugar) builds up in your bloodstream. This can cause you to feel tired and run down or get sick.
There are 2 types of hyperglycemia:
- Acute hyperglycemia happens when a person’s blood glucose spikes suddenly over a period of days or weeks.
- Chronic hyperglycemia happens when a person’s blood glucose rises slowly over a long period of time.
Causes of hyperglycemia
Hyperglycemia can happen if your body doesn’t make enough insulin or can’t easily use the insulin it makes. Insulin is a hormone that lets glucose go from your bloodstream into your cells. If your body does not have enough insulin, glucose stays in your bloodstream and causes hyperglycemia.
Treatment-related hyperglycemia
Some cancer treatments can raise your blood glucose and cause hyperglycemia, including chemotherapy and steroid treatment. Getting nutrition from tube feedings or total parenteral nutrition (TPN) can also cause hyperglycemia.
You may need to keep your blood glucose within a certain range during certain treatments. Your diabetes healthcare provider may prescribe insulin or oral (by mouth) diabetes medicine to improve your glucose levels. They will also explain how to check your blood sugar and how often.
Treatment-related hyperglycemia usually goes away after treatment ends. If it doesn’t, you may have had blood glucose issues before treatment. Keep checking your blood glucose and taking your medicine until your diabetes healthcare provider tells you to stop.
Risk factors for hyperglycemia
Hyperglycemia is more likely to happen if you:
- Have type 1 or type 2 diabetes mellitus (DM) or pre-DM.
- Are not getting enough diabetes medicine to control your blood glucose levels.
- Are not injecting insulin correctly.
- Are using expired insulin or insulin that has gone bad. This can happen if insulin gets too hot or too cold.
- Have not been active enough.
- Eat too many carbohydrates. Read How To Manage Your Blood Glucose (Blood Sugar) With Your Diet to learn more.
- Are getting nutrition from tube feedings or TPN.
- Are sick or have an infection.
- Have physical stress, such as an injury or surgery.
- Have emotional stress, such as from treatment or problems in your personal life.
- Have had all or part of your pancreas removed.
-
Are taking certain medications. Examples include:
- Steroids, such as prednisone or dexamethasone (Decadron®).
- Immunosuppressants, such as tacrolimus and sirolimus.
- Certain types of chemotherapy, targeted therapy, immunotherapy, or hormone therapy. Talk with your healthcare provider to learn more.
Signs and symptoms of hyperglycemia
Your body’s cells need glucose for energy to work as they’re supposed to. For example, if the cells in your muscles don’t have energy, you may feel tired and run down. If your white blood cells don’t have energy, your body can struggle to fight off infection.
The signs and symptoms of high blood sugar can vary from mild to severe (very bad). They may happen acutely (suddenly) if there is a specific trigger. These include developing type-1 diabetes mellitus (T1DM) or steroid-induced hyperglycemia (high blood sugar caused by steroids).
For people with type-2 diabetes mellitus (T2DM), symptoms usually start out mildly and develop slowly over a long time. Mild signs and symptoms can be hard to recognize and may not feel the same to everyone. Because of this, it can take many years to notice or diagnose T2DM.
Acute hyperglycemia
Acute hyperglycemia happens suddenly. Signs and symptoms of acute hyperglycemia include:
- Feeling very thirsty.
- Having a dry mouth.
- Feeling like you need to urinate (pee) often.
- Having dry skin.
- Feeling more hungry than usual.
- Having blurry vision.
- Feeling drowsy.
Severe hyperglycemia
Acute hyperglycemia can get worse if it is not treated. This can lead to a diabetes emergency, such as diabetic ketoacidosis (DKA).
DKA can be life-threatening. If you have DKA or think you have DKA, seek medical attention right away. Call your diabetes healthcare provider, go to your local emergency room, or call 911. Read Diabetic Ketoacidosis (DKA) and Ketone Urine Testing to learn more.
Signs and symptoms of DKA include:
- Feeling confused.
- Feeling shortness of breath.
- Having a dry mouth.
- Feeling weak.
- Having abdominal (belly) pain.
- Feeling nauseous (like you’re going to throw up) or vomiting (throwing up).
- Falling into a coma.
Chronic (long-term) hyperglycemia
Chronic hyperglycemia develops over a long time. Signs and symptoms of chronic hyperglycemia include:
- Having wounds that heal more slowly than usual.
- Getting worse infections or infections more often than usual.
- Having little to no energy.
- Neuropathy (tingling or losing feeling in your fingers and toes).
- Skin changes, such as acanthosis nigricans (AK-un-THOH-sis NI-gruh-KANZ). These are dark, thick areas of soft skin. They usually form on the back of the neck, armpits, or groin area.
- Gum disease. Signs of this include red, sore, irritated gums.
- Any or all of the signs and symptoms of acute hyperglycemia.
How to prevent hyperglycemia
Check your blood glucose
Knowing your blood glucose level is the first step to preventing hyperglycemia. Checking your blood glucose tells you if your glucose levels within your target range. The target range is when your glucose is not too high or too low.
Your diabetes healthcare provider or educator will:
- Tell you how often to check your blood glucose.
- Set your target range based on your health and treatment plan.
- Use your blood glucose readings to adjust your medications as needed.
What is a safe blood glucose range?
MSK’s target blood glucose range for people getting cancer care is usually 100 to 200 milligrams per deciliter (mg/dL). Your diabetes healthcare provider may have different recommendations for you.
How to check your blood glucose at home
You can check your blood glucose level at home using one of these devices:
- A blood glucose meter (or glucometer). You can buy a blood glucose meter at your local pharmacy with or without a prescription. Read How to Check Your Blood Glucose (Blood Sugar) Using a Blood Glucose Meter to learn more.
- A continuous glucose monitor (CGM). Read About Your Continuous Glucose Monitor (CGM) to learn more.
Keep track of your blood glucose results and medicine
Keep track of your blood glucose results and doses of insulin on a blood glucose log. This will help your diabetes healthcare provider safely adjust your medications.
Practice a healthy and active lifestyle
The best way to prevent hyperglycemia and manage your blood glucose is to practice a healthy and active lifestyle. Use your blood glucose readings to guide lifestyle choices to reach your target range. Talk with your diabetes healthcare team about how to do this safely.
Here are some tips for managing your blood glucose levels at home:
Follow a healthy diet
Follow a healthy diet and stay on your meal plan. We recommend following a consistent carbohydrate meal plan, which means having a certain amount of carbohydrates for each meal. Read How To Manage Your Blood Glucose (Blood Sugar) With Your Diet to learn more.
Stay well-hydrated
Drink enough liquids to stay hydrated. Follow your healthcare provider’s instructions for how much liquid to drink.
Drink sugar-free liquids
Drink sugar-free, flavored water, sparkling water (seltzer) or other zero-calorie drinks. Avoid regular soda and fruit juice made with real fruit. These usually have a lot of sugar and can raise your blood glucose.
Get enough physical activity
Physical activity can help keep your blood glucose at a healthy level. Follow your healthcare provider’s instructions on how much activity is safe for you.
Take your diabetes medicine as prescribed
Follow your diabetes healthcare provider’s instructions for taking your diabetes medicine. They will help you plan for what to do if you miss a dose of your medicine.
When to call your diabetes healthcare provider
MSK recommends talking with your diabetes healthcare provider within 10 days after leaving the hospital. Call them if:
- You have new hyperglycemia.
- You were just diagnosed with diabetes.
- Your diabetes medicines have changed.
- Your blood glucose has been above your target range most of the time over the past 2 to 3 days.
- Your blood glucose is lower than 70 mg/dL or higher than 400 mg/dL. These can be dangerous.
- You’re vomiting, or you have diarrhea more than 3 times in 24 hours (1 day).
- You have DKA or think you have DKA.
- You do not feel well and are unsure if you should take your diabetes medications.
- You have a fever of 101° F (38.3° C) or higher.
Go to your local emergency room or call 911 if you cannot contact your healthcare provider right away.
About Hypoglycemia (Low Blood Sugar)
This information explains what hypoglycemia (HY-poh-gly-SEE-mee-uh) is and what signs to look for. It explains how to treat it and how to prevent it from happening.
What is hypoglycemia?
Hypoglycemia is when your blood glucose (blood sugar) level goes too low. This usually happens when your blood glucose goes below 70 milligrams per deciliter (mg/dL).
Your body uses glucose as its main source of energy. If there isn’t enough glucose in your bloodstream, you may have trouble thinking clearly and doing your usual tasks safely. This can happen if you have not eaten enough or are more active than usual.
It is important to treat hypoglycemia right away. If you take medication for diabetes, your healthcare provider may need to change the dosage. Contact the provider who prescribes your diabetes medication any time you have hypoglycemia.
Signs of hypoglycemia and what to look for
Some people show different warning signs when their blood glucose is low. Others may show no signs at all.
Warning signs of hypoglycemia include:

Check for hypoglycemia by measuring your blood glucose at home. Read How to Check Your Blood Glucose (Blood Sugar) Using a Blood Glucose Meter for more information. You can also watch How To Check Your Blood Glucose (Blood Sugar) Using a Blood Glucose Meter.
How to treat hypoglycemia
Follow the rule of 15/15 if your blood sugar is below 70 mg/dL and you’re awake and alert.
Rule of 15/15
- Have 15 grams of sugar. If your blood sugar is below 70 mg/dL, have a simple, rapid-acting sugar. These are foods and drinks that have glucose, dextrose, or sugar listed as the main ingredient. They have little to no (zero) fat or protein. Your body can absorb these items faster. This helps to bring your blood sugar up quickly.
Choose one of these rapid-acting sugars in these amounts:
- Chew 4 large glucose tabs. You can buy these at your local pharmacy without a prescription.
- Drink 4 ounces of fruit juice or soda (not diet soda).
- Chew 5 to 6 gummy candies or hard candies, such as LifeSavers®.
- Have 1 tablespoon of honey or syrup (not sugar-free syrup).
Do not eat chocolate, cookies, or a regular meal or snack to treat low blood glucose. Your body does not absorb these items very quickly. They may make your blood glucose even lower at first, then too high 1 to 2 hours later.
- Wait 15 minutes, then re-test your blood sugar. Re-test your blood sugar after 15 minutes. If your blood glucose is still less than 70 mg/dL, have another 15 grams of sugar. Re-test again 15 minutes later. Keep doing this until your blood glucose level is 70 mg/dL or higher.
Once your blood sugar is 70 mg/dL or higher, have your next meal or small snack within 1 hour. For example, a small snack may include one of the following:
- Peanut butter or cheese with 4 to 5 crackers.
- Half of a sandwich and 4 ounces of milk.
- A single-serve container of Greek yogurt.
What is severe hypoglycemia?
Hypoglycemia can get worse if you do not treat it quickly. Severe hypoglycemia happens when your blood glucose level goes below 54 mg/dL, or when you cannot take care of yourself.
Symptoms of severe hypoglycemia can include:
- Feeling very confused.
- Having trouble following directions or doing simple, routine tasks.
- Trouble speaking or slurred speech.
- Blurry vision or seeing double.
- Loss of balance or trouble walking.
- Suddenly feeling very weak or sleepy.
Talk with your family and friends about the signs of low blood sugar. Teach them what to do if you feel faint or become confused. If you become unconscious (pass out), someone must call 911 for an ambulance.
How to treat severe hypoglycemia
If your blood sugar is below 54 mg/dL, have 24 grams of simple, rapid-acting sugar instead of 15 grams. Choose one of these:
- Chew 6 large glucose tabs. You can buy these at your local pharmacy without a prescription.
- Drink 6 ounces of fruit juice or soda (not diet soda).
- Chew 8 to 9 gummy candies or hard candies, such as LifeSavers®.
- Take 1 ½ tablespoons of honey or syrup (not sugar-free syrup).
Wait 15 minutes, then re-test your blood glucose. Keep doing this until your blood glucose level is 70 mg/dL or higher.
Once your blood sugar is 70 mg/dL or higher, have your next meal or small snack within 1 hour. For example, you can choose to eat one of the following:
- Peanut butter or cheese with 4 to 5 crackers.
- Half of a sandwich and 4 ounces of milk.
- A single-serve container of Greek yogurt.
Emergency glucagon treatments
An emergency glucagon treatment is a prescription medication used to treat severe hypoglycemia. Your healthcare provider may prescribe this if you are at a very high risk for severe hypoglycemia.
If your healthcare provider prescribed an emergency glucagon treatment, read About Emergency Glucagon Treatments for more information.
How to prevent hypoglycemia
It is always best to prevent hypoglycemia before it happens. You can usually do this by balancing your medications, what you eat, and your level of activity. Keeping this balance isn’t always easy. Your provider, diabetes educator, and dietitian can work with you to lower your risk of hypoglycemia.
Follow these steps to lower your risk of hypoglycemia:
- Check your blood sugar more often, especially if you have had hypoglycemia before.
- If you take diabetes medications, be sure to eat enough. Do not skip meals.
-
Talk with your provider before:
- Changing your medications.
- Starting a new exercise routine. Exercise causes your body to use extra glucose.
- Changing how much you eat.
- If you drink alcohol, talk with your healthcare provider about how to do so safely.
When to call your healthcare provider
Call your healthcare provider any time you have hypoglycemia. They may need to change your medication.
About Insulin for Diabetes and Treatment-Related Hyperglycemia
This resource explains what insulin is, how it works, and different types of insulin. It also explains what type 1 and type 2 diabetes are and how to manage them. It answers common questions about insulin and diabetes.
About insulin
Insulin is a hormone that lets glucose (sugar) go from your bloodstream into your cells. Your pancreas makes insulin and releases it into your bloodstream.
Your cells need glucose for energy. If your body does not have enough insulin, glucose stays in your bloodstream. This causes hyperglycemia (high blood sugar).
Hyperglycemia can make you feel tired or sick. It can also make it harder for your body to fight off infection. Read About Hyperglycemia (High Blood Sugar) to learn more.
About type 1 and type 2 diabetes
Type 1 diabetes mellitus (T1DM) is when your pancreas does not make insulin at all.
Type 2 diabetes mellitus (T2DM) is when your pancreas does not make enough insulin. Your pancreas may make less insulin over time. You may also have insulin resistance. This means your cells do not respond to the insulin your body makes. This causes glucose to stay in your bloodstream instead of entering your cells.
How to manage type 1 and type 2 diabetes
People with T1DM must always take exogenous (ex-AH-jin-us) insulin. Exogenous insulin is medicine you inject (take as a shot). It acts like insulin and replaces the insulin your body cannot make.
People with T2DM may need oral medicine (medicine you swallow) to help manage blood glucose levels. As your pancreas makes less insulin over time, you may also need exogenous insulin.
Some diabetes medicines make your pancreas release more insulin. But these medicines will not work if your pancreas cannot make any more insulin. If so, you’ll need to use exogenous insulin to control your blood glucose levels. Talk with your diabetes healthcare provider about how to manage your blood glucose.
When to take insulin
It’s important to take insulin at the right time. Your diabetes healthcare provider will tell you how much to take and when to take it. Taking doses of insulin and other diabetes medicine too close together can raise your risk for hypoglycemia (low blood sugar). Read About Hypoglycemia (Low Blood Sugar) to learn more.
It helps to make a routine for taking insulin. If you miss a dose of insulin, wait until your next scheduled dose. Do not take a dose to make up for a missed dose unless your diabetes healthcare provider tells you to.
What to discuss with your diabetes healthcare provider
Share important health information with your diabetes healthcare provider.
- Had an allergic reaction to diabetes medicines in the past.
- Have liver or kidney problems.
- Have blurry vision or vision changes that make it hard to see clearly.
- Have a severe (very bad) infection.
- Are being treated for heart failure or recently had a heart attack.
- Have problems with your circulation (blood flow). This includes neuropathy (tingling or losing feeling in your fingers and toes).
- Have trouble breathing.
- Drink alcohol.
Types of insulin
Rapid-acting insulin
Rapid-acting insulin starts working within about 15 minutes to lower your blood glucose. It can be used to lower your blood glucose during meals. It can also be used to treat high blood glucose when you’re not eating.
A dose of rapid-acting insulin lasts for about 4 hours.
Examples of rapid-acting insulin include:
- Aspart (Novolog®, Fiasp®)
- Lispro (Humalog®, Lyumjev™)
- Glulisine (Apidra®)
Taking insulin doses too close together can cause hypoglycemia. Take doses of rapid-acting insulin at least 4 hours apart. If your diabetes healthcare provider gives you different instructions, follow their directions.
Mealtime insulin dose
When you eat, your blood glucose rises fast. Rapid-acting insulin is often called a mealtime insulin dose because it manages your blood glucose during meals. If you wait too long to eat after taking your mealtime insulin dose, this can cause hypoglycemia.
Take your mealtime insulin dose no more than 15 minutes before a meal. It’s best to wait until your meal is in front of you and you’re ready to eat. This helps prevent hypoglycemia.
Correctional insulin dose
A correctional insulin dose is when rapid-acting insulin is used to treat high blood glucose levels when you’re not eating. This dose is usually lower than a mealtime insulin dose.
Short-acting insulin
Short-acting insulin can take up to 1 hour to start working and lasts for 6 to 8 hours. If you’re taking it before a meal, take it 30 minutes before you eat. This gives the insulin enough time to start working.
Examples of short-acting insulin include regular human insulin (Humulin R and Novolin® R).
Intermediate-acting insulin
Intermediate-acting insulin usually takes about 2 hours to start working. It lasts for about 12 hours. Intermediate-acting insulin is often used to manage steroid-induced hyperglycemia. This is hyperglycemia caused by steroids, such as prednisone or dexamethasone.
If you’re taking intermediate-acting insulin for steroid-induced hyperglycemia, take the insulin and the steroid together. Do not take the insulin without taking the steroid unless your diabetes healthcare provider tells you to.
Tell your diabetes healthcare provider if your steroid dose changes, is held, or stopped suddenly. They may need to stop or adjust your insulin dose.
Examples of intermediate-acting insulin include Neutral Protamine Hagedorn insulin (Humulin N and Novolin® N). Neutral Protamine Hagedorn is also called NPH.
Long-acting insulin
Long-acting insulin is also called basal insulin or background insulin. Long-acting insulin works slowly over a long period of time. It works to keep glucose levels stable when you’re not eating, such as between meals or while you sleep. Long-acting insulin is not used to control the quick rise in glucose caused by eating.
Long-acting insulin starts working in about 2 hours. Some insulin lasts 20 to 24 hours. These include glargine (Lantus®, Basaglar®, Semglee®, and Rezvoglar™). Other insulin, such as insulin glargine U-300 (Toujeo®) and insulin degludec (Tresiba®), lasts 36 to 42 hours.
Take long-acting insulin at the same time every day unless your diabetes healthcare provider gives you other instructions. It’s helpful to set an alarm or reminder on your smartphone.
Common questions about diabetes and insulin
Will I become addicted to or dependent on exogenous insulin?
No. Taking exogenous insulin injections (shots) does not cause your body to make less insulin. If your body makes insulin, it will keep making it just the way it did before.
You can use exogenous insulin for short periods of time, such as during treatment.
Certain medicines cause hyperglycemia, but only while you’re taking them. These include steroids and some chemotherapies. Once you finish the treatment with these medicines, your blood glucose goes back to what it was before.
Tell your diabetes healthcare provider if your dosage of steroids or chemotherapy changes. You may need to change how much insulin you take, too. Follow your diabetes healthcare provider’s instructions.
What are the side effects of exogenous insulin?
Exogenous insulin is very similar to the insulin your body makes. This means it does not have many side effects.
The most common side effect of exogenous insulin is hypoglycemia. You can prevent this by taking your insulin as prescribed, knowing your blood glucose levels, and not skipping meals.
Tell your healthcare provider if you develop a rash. This is rare but may be a sign of an allergy.
Why can’t I just take a pill?
Oral diabetes medicine will only help your body do the things it usually does better. It cannot make your body do something it cannot already do. For example, if your pancreas cannot make more insulin, you may need to take insulin injections. Read About Oral and Non-Insulin Injectable Diabetes Medicine to learn more.
Can taking exogenous insulin cause problems with my eyesight? Can it affect how well my kidneys work? Can it make me lose my fingers, toes, or legs?
Some people do not want to start insulin until they can no longer delay taking it. But waiting too long can cause other health problems. Uncontrolled high blood glucose over long periods of time can cause eyesight loss. It can affect how well your kidneys work. You may lose your fingers, toes, and legs.
It’s best to manage your blood glucose right away, before other health problems start.
You may have vision changes as insulin brings your blood glucose under control. Tell your healthcare provider if this happens.
Is it my fault that I need to take insulin? Did I not take good enough care of myself?
Your genetics are one of the main causes of diabetes. Over time, diabetes lowers your body’s ability to make enough insulin. This is mostly out of your control. It is not your fault that your body loses cells that make insulin. Eating too much sugar does not cause you to have diabetes.
How to Improve Your Blood Sugar With Your Diet
This information explains how to manage your blood glucose with your diet. It also explains how to manage cancer treatment side effects and your blood glucose at the same time.
About blood glucose and your diet
Glucose is a simple sugar. It is the main source of energy for cells and comes from the foods you eat. Many things can affect your blood glucose, such as:
- Stress.
- Medicine.
- Changes to your diet.
- Physical activity and exercise.
Some cancer treatments and their side effects can also make your blood glucose levels go up or down. Managing your blood glucose is an important part of your cancer care, and we’re here to help.
A big part of managing your blood glucose is understanding what to eat. This can feel overwhelming. A clinical dietitian nutritionist or diabetes educator can help you to create a plan that is best for you. They will base their recommendations on your health and health goals. If you’d like to talk with a clinical dietitian nutritionist or diabetes educator, ask your healthcare provider.
The best diet is personal and different for every person. Your ideal diet is based on your health, cancer treatment plan, blood glucose goals, and personal preferences. It’s also important to try to follow a well-balanced diet that gives you the nutrients your body needs.
About carbohydrates
There are 3 main types of nutrients:
- Carbohydrates, also called carbs.
- Fats.
- Proteins.
These main nutrients are sometimes called macronutrients or macros. Many foods have all three of these nutrients. Each of these nutrients can turn into glucose, but this process is much easier and faster with carbohydrates. This is why your body uses carbohydrates as its main source of energy.
The following table has examples of foods and drinks with carbohydrates and foods without carbohydrates.
| Foods with carbohydrates | Foods without carbohydrates |
|
|
How carbohydrates affect your blood glucose
It’s important to include carbohydrates in your diet. Your body breaks down carbohydrates into glucose. Glucose is then released into the bloodstream where your cells can use it for energy.
While carbohydrates give your body energy, they also affect your blood glucose levels. Not all carbohydrates raise your blood glucose the same way. Some raise your blood glucose levels very quickly, while others raise them more slowly (see Figure 1). This can make it hard to manage your blood glucose.

Eating too many carbohydrates can increase your risk of high blood sugar (hyperglycemia). It’s important to keep your blood glucose from getting too high or too low (hypoglycemia).
The amount of carbohydrates you need is different for each person. For example, if you have type 1 diabetes mellitus (T1DM), you must have carbohydrates in your diet. Your healthcare provider will work with you to figure out your blood glucose goals and carbohydrate needs.
Your healthcare provider or diabetes educator will set your blood glucose target numbers. Keeping your blood glucose near those target numbers is an important part of your treatment.
About dietary fiber
Fiber is a type of carbohydrate. It slows down how quickly your body absorbs sugar. This helps manage your blood glucose levels.
There are two different types of fiber:
- Soluble fiber breaks down in water to form a gel. It is easier for your body to digest. Soluble fiber helps control blood glucose levels by slowing down how fast your body uses carbohydrates.
- Insoluble fiber does not dissolve in water. Because of this, it can help move stool (poop) through your body.
Tips to help you manage your blood glucose with your diet
Manage your blood glucose with carbohydrates
Here are some ways to manage the amount of carbohydrates you have in your diet.
Plate method
To help control carbohydrate portions, it can be helpful to follow the plate method. To do this:
- Fill ½ your plate with non-starchy vegetables, such as spinach, broccoli, or peppers.
- Fill ¼ of your plate with lean proteins, such as chicken, turkey, or seafood, including shellfish.
- Fill ¼ of your plate with high fiber carbohydrates, such as brown rice, sweet potatoes, or quinoa.
Limit the amount of carbohydrates in your meals, when needed
If your blood glucose is high, having meals with fewer carbohydrates can help bring it back to your target range. Never stop eating all carbohydrates, especially if you take insulin. This can make your blood glucose go too low. Talk with your healthcare provider for more information.
Here are some ways to have less carbohydrates in your meals:
- Have 1 main source of carbohydrate in your meal instead of 2. For example, have either whole grain rice or beans instead of both.
- Have an open-faced sandwich on one slice of bread instead of two.
- Drink sugar-free, flavored water and sparkling water instead of fruit juice or soda. Fruit juice made with real fruit usually has a lot of sugar.
- Substitute or add more protein, such as an egg, to your breakfast instead of having more bread or fruit.
- Limit refined grains, such as boxed pastas or some cereals.
- Choose whole foods instead of processed foods when you can. For example, choose apples instead of applesauce.
For people taking diabetes medicine
If you take diabetes medicine, talk with your healthcare provider or diabetes educator before lowering the amount of carbohydrates you eat and drink. If you lower the amount of carbohydrates you eat by too much, you could be at risk for low blood glucose (hypoglycemia). To learn more, read About Hypoglycemia (Low Blood Sugar).
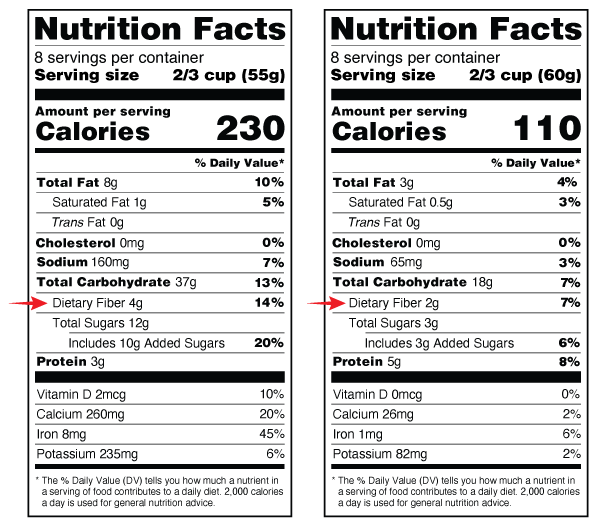
Counting carbohydrates to manage your blood glucose
Carbohydrate counting is when you plan and track meals that have a certain number of grams of carbohydrates per meal. Carbohydrate counting helps you manage your blood glucose levels with the food you eat. This type of meal plan is often recommended for people taking insulin.
When you’re counting carbohydrates, use the number in the “Total Carbohydrate” row in the Nutrition Facts label (see Figure 2). Aim for 45 to 60 grams total carbohydrate at each meal. If your endocrinologist or diabetes educator recommends a different amount, follow their instructions. See the “Sample menus” section at the end of this resource for ideas for meals that meet these carbohydrate goals.

During your treatment, your doctor may ask you to track or change the amount of carbohydrates in your diet. This is to help manage your blood glucose levels. Always talk with your clinical dietitian nutritionist, diabetes educator, or doctor before changing the amount of carbohydrates in your diet.
Difference between grams listed on Nutrition Facts labels
Sometimes both the serving size and the amount of carbohydrates in a serving can be measured in grams. But they are not the same.
- Grams (g) listed next to the “Serving Size” tells you the weight of the food item in grams. If you are using a food scale, you can use this information to measure the serving size (see Figure 3).
- Grams (g) listed next to “Total Carbohydrate” tells you the amount of carbohydrate in one serving of the food (see Figure 3).

Steps to carbohydrate counting
Step 1: Talk with your care team to decide the amount of carbohydrates you should have at each meal.
Step 2: Include foods in your meal that have carbohydrates. Use examples in the “About carbohydrates” section of this resource. Talk with a clinical dietitian nutritionist or diabetes educator to learn more.
Step 3: Calculate the grams of carbohydrates (per serving) for the food you’re eating. To do this, use the Nutrition Facts label to find the serving size and total grams of carbohydrates per serving (see Figure 3).
Step 4: Calculate the total amount of carbohydrates by adding the grams from each source of carbohydrate. For example, a serving of Cheerios and 1 cup of 1% milk has 41 grams of carbohydrates (see Figure 4).

Carbohydrates in 1 serving size (1 ½ cups or 32 g) of Cheerios = 29 g
Carbohydrates in 1 serving size (1 cup) of 1% low fat milk = 12 g
Total carbohydrates (29 g + 12 g) = 41 g
Step 5: Measure your foods to the serving size on the food label (see Figure 4). You can use a measuring cup or a kitchen scale. It’s important to measure your food initially so that you get used to what the serving size is. But after you become used to what the serving size looks like, it’s OK to estimate your measurements. They don’t need to be exact. Talk with your clinical dietitian nutritionist for more information about measuring your serving sizes.
What to do if you do not have a Nutrition Facts label
If a food does not have a Nutrition Facts label or you’re eating out, search for the carbohydrate information online. Some websites, such as www.CalorieKing.com and www.MyFitnessPal.com, also have mobile applications (apps) for your smartphone or tablet. Talk with a clinical dietitian nutritionist for more resources.
For people taking insulin
If you’re taking insulin, your healthcare provider can show you how to measure your insulin dose for each meal. Talk with your healthcare provider or diabetes educator for more information.
How to manage your blood glucose with fiber
Another way to manage your blood glucose is to choose carbohydrates that have more fiber and less sugar. Choose foods with more than 3 grams (g) of fiber per serving. These include foods such as foods such as oats, peas, beans, apples, citrus foods, and barley.
It’s important to eat high-fiber foods that have soluble fiber, such as:
- ¾ cup to 1 cup serving of multi-grain cereal.
- ½ cup of cooked beans or lentils.
- 3 cups of air popped popcorn.
- 1 medium potato or sweet potato.
It can be hard to only eat carbohydrates that are high in fiber. Try to switch out low-fiber foods with high-fiber foods as often as you can.
You can find the amount of fiber in packaged foods by reading the Nutrition Facts label. The Nutrition Facts label has information about the amount of certain nutrients in the food or drink. The amount of fiber is listed in the “Dietary Fiber” row (see Figure 5).
How to manage nutrition during cancer treatment
During cancer treatment, side effects can limit your ability to eat well. Side effects can include nausea (feeling like you’re going to throw up), taste changes, or appetite loss (not wanting to eat).
Being unable to eat can raise your risk for weight loss. It also raises your risk for malnutrition (when your body does not get all the nutrients it needs).
Read Eating Well During Your Cancer Treatment to learn more about general nutrition guidelines during cancer care.
If you’re having a hard time eating during treatment, talk with your healthcare providers and clinical dietitian nutritionist. You may need to change your diet to get the nutrients you need. Sometimes, they may want you to focus less on carbohydrate counting.
Eating small meals more often can make it easier to meet your nutrition goals. Your clinical dietitian nutritionist can help set your carbohydrate goals for each smaller meal. Focus on eating more protein and healthy fats. This will help you get the nutrients you need as you manage your blood glucose.
Here are some examples of foods with proteins and healthy fats:
- Nuts and nut butters.
- Seeds, such as pumpkin seeds or flax seeds.
- Avocados.
- Unsweetened (plain) yogurt and cheese.
- Lean protein, such as fish, chicken, eggs, and tofu.
- Olive oil and canola oil.
Diet changes can help. But you still may need medicine to manage side effects better. If you’re prescribed medicine, be sure to follow your care team’s instructions for taking them.
How to manage loss of appetite during cancer treatment
Appetite loss means you have less of a desire to eat. It’s a very common side effect of treatment. When you lose your appetite, you may want to eat comfort foods to feel better. This can make it harder to eat a well-balanced diet and manage your blood glucose levels.
Try these tips to help you get the most from your meals when you can’t eat much:
- Add more protein to your diet, such as chicken, fish, eggs, or tofu.
- Have a protein shake or nutritional supplement that’s high in protein and low in carbohydrates. Some are high-calorie, ready-made drinks that have vitamins and minerals added to them. Others are powders that you can mix into other foods or drinks. Most are also lactose-free. That means you can have them even if you’re lactose intolerant (have trouble digesting milk products). Talk with a clinical dietitian nutritionist for suggestions.
- Talk with your healthcare provider about your symptoms. They may give you a prescription for a medicine to help with your appetite.
It’s hard to manage your blood glucose while going through cancer treatment. Sometimes you need more than the right diet and exercise routine. If you’re having trouble managing your blood glucose, talk with your care team.
Sample menus
Your care team may tell you to aim for 45 to 60 grams of carbohydrates per meal. Follow your care team’s instructions. Do not eat more than 60 grams of carbohydrates at any meal.
Aim to have about the same mount of carbohydrates at each meal:
- 3 to 4 servings (45 to 60 grams) of carbohydrates for breakfast.
- 3 to 4 servings (45 to 60 grams) of carbohydrates for lunch.
- 3 to 4 servings (45 to 60 grams) of carbohydrates for dinner.
Below are sample menus with ideas for meals and snacks that meet these carbohydrate goals. These menus are meant to be examples. Each menu shows how many grams of carbohydrates are in each item.
| Meal Time | Sample menu 1 | Sample menu 2 |
Breakfast (based on 45 to 60 g carbohydrates)
| 1 small orange (15 g) ½ avocado (10 g) 2 scrambled eggs (0 g) 1 whole wheat English muffin (22 g) 1 teaspoon butter (0 g) 1 cup coffee (0 g) | 2 cups Cheerios (40 g) 1 cup 1% milk (12 g) 1 tablespoon peanut butter (0 g) 1 cup coffee (0 g) |
| Lunch (based on 45 to 60 g carbohydrates) | 4-ounce hamburger (0 g) 1 slice of American cheese (0 g) 1 slice lettuce, tomato (1 g) 1 hamburger bun (22 g) 1 small apple (15 g) 1 ounce salted hard pretzels (22 g) 1 cup water (0 g) | 4 oz. turkey (0 g) 1 slice lettuce, tomato (1 g) 2 slices rye bread (32 g) 1 ounce snack pack of baked Lays chips (24 g) 12 ounces seltzer with lime slice (0 g) |
| Dinner (based on 45 to 60 g carbohydrates) | 4 ounces baked chicken with breading (10 g) 1 white cup rice (44 g) 2 cups broccoli (0 g) 12 ounces seltzer (0 g) | 2 ounces cooked ziti pasta (44 g) ½ cup tomato basil sauce (10 g) 2 cups tossed salad (0 g) 1 cup mixed raw salad veggies (0 g) 1 tablespoon oil (0 g) 1 tablespoon vinegar (0 g) |
About Emergency Glucagon Treatments
This information explains what glucagon is and how to be prepared for an emergency. It also has instructions for caregivers who may need to give an emergency glucagon treatment.
- Glucagon (GLOO-kuh-gon) is a hormone that tells your liver to release stores of sugar into your bloodstream. This helps raise your blood sugar quickly.
- Hypoglycemia (HY-poh-gly-SEE-mee-uh) is blood sugar that’s too low.
-
Severe hypoglycemia is when either of these things happens:
- Your blood sugar level goes below 54 milligrams per deciliter (mg/dL).
- You feel faint, weak, or confused and cannot care for yourself because your blood sugar is too low.
About emergency glucagon treatments
An emergency glucagon treatment is a medication used to treat severe hypoglycemia. Your liver stores sugar to use as energy or to raise low blood sugar. An emergency glucagon treatment tells your liver to release the sugar into your bloodstream. This helps raise your blood sugar back to normal levels (70 mg/dL).
Read About Hypoglycemia (Low Blood Sugar) for more information about hypoglycemia and how to treat it.
When to use an emergency glucagon treatment
It’s best to treat hypoglycemia by eating or drinking a rapid acting sugar, such as juice or glucose tablets. Rapid acting sugars are foods and drinks that have glucose, dextrose, or sugar listed as the main ingredient. If you cannot eat or drink, use an emergency glucagon treatment.
If you become confused, you may need someone else to give you the treatment. Share this information with family members, friends, and coworkers ahead of time. They will need to know what to do to help you in case of an emergency. Have them read the “A Caregiver’s Guide to Emergency Glucagon Treatments” section of this resource for more information.
How to prepare yourself to use emergency glucagon treatments
Talk with your healthcare provider
Tell your healthcare provider if you have:
- Pheochromocytoma (FEE-oh-KROH-moh-sy-TOH-muh). This is a small tumor on the adrenal gland.
- Insulinoma (IN-suh-lih-NOH-muh). This is a tumor that secretes insulin.
- Glucagonoma (GLOO-kuh-guh-NOH-muh). This is a tumor that secretes glucagon.
Tell your healthcare provider if you cannot eat or drink for one week or longer. This may cause the sugar stored in your liver to become low. When this happens, glucagon may not work as well. You may need to get dextrose (a form of sugar) through an intravenous (IV) line to treat hypoglycemia.
Store your emergency glucagon treatment
Keep your emergency glucagon treatment at room temperature (68 °F to 77 °F or 20 °C to 25 °C). Do not refrigerate or freeze it. Keep it in the container it came in, tightly closed. Tell your family, friends, and coworkers where you keep your treatment stored.
Check the expiration date on your glucagon treatment
Set an alarm or mark your calendar to remind you to check the expiration date regularly. Get a new prescription from your healthcare provider and replace it before it expires.
A Caregiver’s Guide to Emergency Glucagon Treatments
This information explains when to use emergency glucagon treatment. It also explains the different types of emergency glucagon treatment kits. Read the “Types of emergency glucagon treatments” section of this resource for more information about their specific treatment.
Do not wait until an emergency to read this information. Be ready for an emergency by doing these things ahead of time:
- Read About Hypoglycemia (Low Blood Sugar).
- Know when and how to use their emergency glucagon treatment.
- Talk with the person about where they keep their emergency glucagon treatment.
When to use an emergency glucagon treatment
You may need to use an emergency glucagon treatment if the person has severe hypoglycemia and cannot take care of themselves. Only use the emergency glucagon treatment if the person cannot eat or drink.
If they are able to safely eat or drink, follow the rule of 15/15. If the person starts to cough or has difficulty swallowing do not give them anything else to eat or drink.
- Give them their emergency glucagon treatment right away.
- Turn them on their side after giving them the treatment. They might vomit (throw up) after getting glucagon. This can be dangerous if they’re lying on their back.
- Call 911 for an ambulance.
What to do after giving someone an emergency glucagon treatment
Check the person’s blood sugar level 15 minutes after the treatment. An unconscious person will usually wake up within 15 minutes.
If the person is awake within 15 minutes
- If their blood sugar is still below 70 mg/dL, follow the rule of 15/15.
-
If their blood sugar is 70 mg/dL or higher, have them eat a snack or next meal within one hour. This will help stop their blood sugar from dropping again. A small snack may include one of the following:
- Peanut butter or cheese with 4 to 5 crackers.
- Half of a sandwich and 4 ounces of milk.
- A single-serve container of Greek yogurt.
If the person is not awake after 15 minutes
- Give them a second emergency treatment, if they have one.
- Wait for emergency services to arrive.
Types of emergency glucagon treatments
There are different types of emergency glucagon treatment devices. It helps to be familiar with the type of device the person has before you need to use it. Follow the instructions that come with the medication.
Gvoke HypoPen®
Gvoke HypoPen is an emergency glucagon injection (shot) device. The injection goes under the skin of the person’s arm, belly, or thigh. An injection that goes under the skin is a subcutaneous (SUB-kyoo-TAY-nee-us) injection.
Gvoke Pre-filled syringe®
Gvoke Pre-filled syringe is an emergency glucagon injection device. The injection goes under the skin of the person’s arm, belly, or thigh. An injection that goes under the skin is a subcutaneous (SUB-kyoo-TAY-nee-us) injection.
BAQSIMI®
BAQSIMI is an emergency glucagon powder. It’s sprayed into the person’s nose, like other nasal sprays.
Emergency glucagon injection kit
An emergency glucagon injection kit is an intramuscular (IN-truh-MUS-kyoo-ler) medication. An intramuscular injection (shot) goes directly into the muscle. Emergency glucagon injection kits do not come ready to use like some other treatments. You will need to get it ready right before you use it.
How to safely get rid of an emergency glucagon treatment kit
Each emergency glucagon treatment device should only be used once. After you use it, throw it away. If the person needs another treatment, use a new device.
Do not throw needles or syringes directly into the trash or flush them down the toilet. Put them into a sharps container or a hard, plastic container with a screw top lid, such as a laundry detergent bottle. Label the bottle by writing “Home Sharps: not for recycling” on it. Read How to Store and Get Rid of Your Home Medical Sharps for more information.
Diabetic Ketoacidosis (DKA) and Ketone Urine Testing
This information describes what diabetic ketoacidosis (DKA) is. It explains how to test for it using a ketone urine test. It also explains the symptoms of DKA and the steps you can take to prevent it.
What is diabetic ketoacidosis?
Causes of diabetic ketoacidosis
DKA is a medical emergency that happens when your body does not have enough insulin. Insulin is a hormone that lets glucose (sugar) go from your bloodstream into your cells. The cells in your body use glucose for energy. Cells need energy to live.
If your body does not have enough insulin, glucose cannot get into your cells. It will stay in your bloodstream where it can cause hyperglycemia (high blood sugar).
If your body cannot use glucose for energy, it uses fat instead. This happens slowly so it can make you feel tired and run down. As your body turns fat into energy, ketones (blood acids) form and enter your bloodstream. Ketones leave your body through your urine (pee).
You can test your body’s ketone levels at home using urine ketone test strips. Read the “Testing your ketone levels” section of this resource for more information.
Ketosis
Ketosis (kee-TOH-sis) is when some ketones build up in your bloodstream. This can happen if you suddenly lose your appetite or lose weight. This is common for people going through treatment for cancer.
Having some ketones in your bloodstream can be normal and does not always mean you have DKA. Talk with your diabetes healthcare provider about what level of ketones is safe, and when to call for medical help.
Some diets, such as the ‘keto diet’, use ketosis as a tool for losing weight. This can be unsafe for people who are ill or have diabetes. Talk with your healthcare provider about whether a keto diet is safe for you.
Ketoacidosis
Ketoacidosis (KEE-toh-A-sih-DOH-sis) is when too many ketones build up in your bloodstream. This makes your blood acidic, which can be dangerous.
Risk factors for diabetic ketoacidosis
You may be at a higher risk for DKA if:
- You have new diagnosis of type 1 diabetes (T1DM). For people with cancer, T1DM can be a rare side effect of some immunotherapy treatments.
- You missed insulin doses, or if your body needs more insulin. Follow your diabetes healthcare provider’s instructions for taking insulin. Never change your insulin dose without talking with your diabetes healthcare provider first.
- Your insulin has expired or has gone bad. This can happen if your insulin gets too hot or too cold.
- Your insulin pump stops working as it should.
- You take steroid medications, such as prednisone or dexamethasone.
- You have an infection or a stressful medical condition. For example, DKA can happen after surgery, which is a stressful procedure.
DKA is more common in people with T1DM. Far less often, DKA can happen if you have type 2 diabetes (T2DM). But at least one of these other things also must be true:
- You have severe pancreatitis (PAN-kree-uh-TY-tis), which is inflammation (swelling) of the pancreas.
- You take steroid medications.
-
You take a sodium-glucose cotransporter-2 (SGLT2) inhibitor medication, or a combination medicine that includes:
- Invokana® (canagliflozin)
- Farxiga® (dapagliflozin)
- Jardiance® (empagliflozin)
- Steglatro® (ertugliflozin)
- Brenzavvy® (bexagliflozin)
Read the “Euglycemic DKA (EDKA)” section of this resource for more information.
Signs and symptoms of diabetic ketoacidosis
DKA often happens quickly, sometimes within a few hours. You may get very sick quickly, even before you notice any symptoms.
Talk with your healthcare provider to make a sick day plan. Follow their instructions for checking your blood glucose and taking diabetes medication when you’re not feeling well. Read How to Manage Diabetes When You’re Sick to learn more.
A high blood glucose level often is one of the first signs of DKA. Other early symptoms of diabetic ketoacidosis are:
- Dry mouth.
- Dry skin.
- Extreme thirst (feeling thirsty even after drinking a lot of fluids).
- Urinating (peeing) often.
If not treated, symptoms of DKA can get worse, including:
- Suddenly feeling weak or tired.
- Nausea (feeling like you’re going to throw up) or vomiting (throwing up).
- Belly pain.
- Confusion or trouble thinking.
- Fruity-smelling breath.
- Trouble breathing.
- Flushed skin (skin that feels warm and is red or splotchy).
Euglycemic DKA (EDKA)
EDKA is a rare condition. This happens when you have DKA, but your blood glucose is normal or near normal (less than 250 mg/dL). Having normal or near normal blood glucose levels can make it easy to miss an EDKA diagnosis.
You are more likely to get EDKA if:
- You take a SGLT2-inhibitor.
- You have T1DM and you miss insulin doses or take too little insulin.
If you take an SGLT2-inhibitor and have any signs or symptoms of DKA, tell your diabetes healthcare provider right away. Do this even if your blood glucose level is normal or near normal.
SGLT2-inhibitors and diabetic ketoacidosis
If you have diabetes, your healthcare provider may prescribe SGLT2-inhibitors. These help your body get rid of extra glucose by causing you to urinate more. This helps lower your blood glucose.
When you urinate more, you may become dehydrated. This can raise your risk of EDKA. Talk with your healthcare provider about drinking more fluids while taking SGLT2-inhibitors.
Your risk of EDKA also goes up if you take SGLT2-inhibitors and:
- You’re eating or drinking less than normal for you. This can happen if you’re fasting before surgery, or have a poor appetite, nausea, or vomiting.
- You had a general surgery or other procedure, such as a colonoscopy.
If you’re having surgery or a procedure, follow your healthcare provider’s instructions for taking an SGLT2-inhibitor. You may need to stop taking it several days ahead of time.
Testing for ketones
Ketones are usually in your urine or blood. They leave your body through your urine. Your healthcare provider may test for ketones in your blood. You can also test your body’s ketone levels at home using urine ketone test strips. You can buy these at your local pharmacy without a prescription.
When to test for ketones
You should test for ketones if any of these things applies to you:
- You have symptoms of DKA.
- Your blood glucose is more than 250 mg/dL right after you wake up and before you’ve eaten.
- Your blood glucose is more than 250 mg/dL for 2 tests in a row, such as before breakfast and lunch.
- You cannot take your usual insulin dose because you are not eating or drinking as you normally would.
- You cannot take your usual insulin dose because you are not feeling well. This includes if you have a cold, infection, nausea, or vomiting.
- You take an SGLT2-inhibitor and are not eating or drinking, even if your blood glucose is less than 250 mg/dL.
How to test your ketone levels
Here are general steps for how to test your ketone levels. Follow the instructions on the bottle or box of test strips if they’re not the same as these steps:
- Collect a fresh urine sample.
- Dip a ketone test strip into the urine sample.
- Wait for the number of seconds it says in the instructions. The color of the pad on the strip will change if there are ketones in your urine.
-
Compare the color of the pad to the color chart on the bottle or box (see Figure 1). The test results will be either negative or positive.
- A negative result means there are no ketones in your urine.
- A positive result means there are ketones in your urine. A positive result is measured as a small, moderate, or high level of ketones.
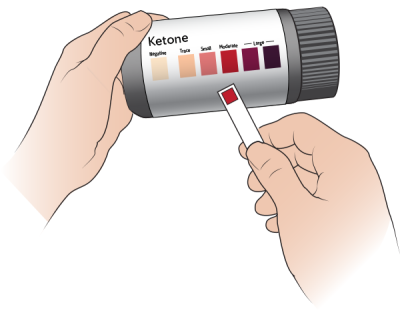
What to do if you your ketone levels are high
- Drink extra water or zero-calorie drinks.
- Avoid sugary drinks, such as juice or soda.
- For people with T1DM, follow your sick day plan. This often includes checking your blood glucose level and testing for ketones every 3 to 4 hours or as instructed.
- Take insulin as instructed.
- If you take an SGLT2-inhibitor, do not take any more doses. Call your diabetes health care provider right away. They will tell you what to do if you have a positive ketone test.
- Do not exercise if your blood glucose is over 250 mg/dL and you have a positive ketone test result.
How to prevent DKA
- Tell your diabetes healthcare provider if your blood glucose levels are over 200 mg/dL for 3 days in a row.
- Always follow your diabetes healthcare provider’s instructions for taking your medications exactly as prescribed.
- Check your blood glucose often. Follow your diabetes healthcare provider’s instructions.
- Never stop eating all carbohydrates without being monitored by your care team. Examples of carbohydrates (carbs) include bread, rice, fruit, and pasta.
- If you take insulin or an SGLT-2 inhibitor, tell your diabetes healthcare provider if you have any surgery or procedures planned.
For people with type 1 diabetes (T1DM)
Create a sick day plan with your diabetes healthcare provider. They may tell you to take small doses of insulin often, even if you cannot eat or drink. Talk with them about any procedures you’re planning to have.
When to call your healthcare provider
Contact your diabetes healthcare provider right away if you have any of the following:
- Your urine test shows moderate to high levels of ketones.
- Your blood glucose levels are higher than 400 mg/dL.
- You’re vomiting, or you have diarrhea more than 3 times in 24 hours (1 day).
- You’re not sure if you should take your diabetes medications because you’re not feeling well.
- A fever of 101° F (38.3° C) or higher.
Go to your local emergency room or call 911 if you cannot contact your healthcare provider right away.
How to Manage Diabetes When You’re Sick
This information has guidelines for managing diabetes when you are not feeling well. It also explains what to do ahead of time, so you have everything you need when you’re sick.
Follow these guidelines if you have:
- A cold.
- Influenza (the flu).
- An infection.
- Any illness, condition, or side effects that make it hard to eat or drink like usual.
What to do before you’re sick
It’s very important to plan ahead. Getting ready before you get sick will make it easier to care for yourself when you don’t feel well.
Make a sick day plan
Talk with your diabetes healthcare provider about what to do if you get sick. Your diabetes healthcare provider is the provider who manages your blood glucose (blood sugar) levels. They can give you a more detailed sick day plan.
The plan for when you’re sick should have instructions for:
- When you should contact them.
- How often to check your blood glucose levels.
- How to take your diabetes medicine.
- Which over-the-counter medicine you can use. Some can raise your blood glucose or affect your usual medicine. Over-the-counter medicine is medicine you buy without a prescription.
- If you should test your urine (pee) for ketones and when to test it.
- When to get emergency medical help.
Keep a list of all your healthcare providers and their phone numbers. Make sure to include how to contact them after business hours.
Stock up on medicine and other supplies
Your blood glucose levels may be higher than usual when your body is under stress. This includes being sick. You’ll need to be even more careful than usual to manage diabetes.
It’s important to keep your blood glucose in your target range, even if you can’t eat or drink. The target range is when your glucose is not too high or too low. You may need more medicine than usual to do this.
Make sure you always have enough medicine and supplies for several weeks or longer. Examples are listed below.
-
Diabetes medicine and supplies, such as:
- Oral diabetes medicine. This is diabetes medicine you swallow.
- Injectable diabetes medicine. This is diabetes medicine you take as a shot.
- Insulin pen needles.
-
Monitoring supplies, such as:
- Blood glucose test strips.
- Lancets.
- Ketone test strips. You’ll need these if:
- You’re at high risk for diabetic ketoacidosis (DKA).
- Your diabetes healthcare provider tells you to test for ketones.
-
Other medicine and supplies, such as:
- A thermometer.
- Medicine for nausea (feeling like you’re going to throw up) that your care team prescribes.
- Medicine for pain and fevers. Examples include acetaminophen (Tylenol®) or ibuprofen (Advil® and Motrin®).
- Medicine for diarrhea (loose or watery poop). Examples include loperamide (Imodium®) or bismuth subsalicylate (Pepto-Bismol® and Kaopectate®).
- Medicine for constipation (having fewer bowel movements than usual). Examples include milk of magnesia (Phillips’® Milk of Magnesia), polyethylene glycol (MiraLAX®), or bisacodyl (Dulcolax®).
- Medicine for heartburn or upset stomach. Examples include antacids (Mylanta® or Maalox®).
Talk with your healthcare provider before taking any over-the-counter medicine. Some can affect the way your usual medicine works.
Stock up on foods and drinks
You should also have some quick and easy foods or meals. Examples are listed below.
- Saltine crackers or pretzels.
- Unsweetened applesauce.
- Instant cooked cereals, such as oatmeal or Cream of Wheat®.
- Canned soups.
- Regular or low-sodium broth from a box, can, or packet.
- Instant pudding or premade pudding cups.
- Regular gelatin (not sugar-free), such as Jell-O®.
- Regular soft drinks, such as ginger ale or Sprite®.
- Diet soft drinks (soft drinks without calories). Examples include diet ginger ale or Sprite Zero Sugar.
- Electrolyte drinks with calories. Examples include Gatorade® or vitaminwater®.
- Electrolyte drinks without calories. Examples include G-Zero or vitaminwater Zero.
- Juice boxes or small cans of fruit juice.
- Tea.
- Nutritional drinks for people with diabetes. Examples include Glucerna® or BOOST Glucose Control®.
What to do when you’re sick
- Follow your diabetes healthcare provider’s instructions for how often to test your blood glucose levels.
- Follow your diabetes healthcare provider’s instructions for taking your diabetes medicine.
- Get plenty of rest.
- Tell a family member or friend that you’re sick. They can check in with you to make sure you’re OK and help you if needed. Make sure they know where to find the list of your healthcare providers and their phone numbers.
Eating and drinking
Try to keep eating and drinking plenty of calorie-free liquids when you’re sick. If you can’t eat normal meals, take small bites of food and sips of liquids often.
Aim to eat or drink about 50 grams of carbohydrates every 3 to 4 hours when you’re awake. Check the nutrition facts label (see Figure 1) to see how many carbohydrates are in a serving. Nutrition facts labels can also help you compare the nutritional information for different products.
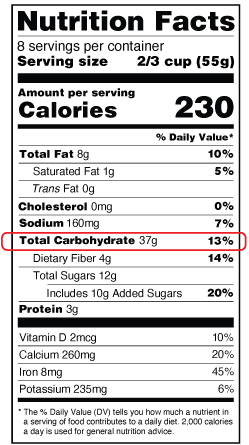
Preventing dehydration
Dehydration is when there aren’t enough fluids in your body. Being dehydrated can lead to kidney failure, even if it’s for less than 24 hours.
Drinking lots of liquids is one of the most important things to do when you’re sick. Aim to drink around 8 to 10 (8-ounce) glasses (about 2 liters) of liquids every day.
If you have any of the following signs of dehydration, contact your healthcare provider right away.
- Dizziness, especially when you stand.
- Urinating (peeing) less than usual.
- Dark, amber-colored urine.
- Feeling more thirsty than usual.
- Headache.
- Muscle cramps.
- Dry mouth or cracked lips.
- A fast, irregular heartbeat.
- Loss of appetite.
When to call your healthcare provider
Call your healthcare provider if:
- You have any signs of dehydration listed above.
- Your blood glucose is less than 70 milligrams per deciliter (mg/dL). Read About Hypoglycemia (Low Blood Sugar) to learn more about how to manage low blood glucose.
- Your blood glucose stays over 250 mg/dL, even after taking higher doses of medicine following your diabetes healthcare provider’s instructions.
- You have a fever of 100.4 °F (38 °C) or higher.
- You’ve vomited every time you drank something in the past 4 hours.
- You’ve had vomiting, diarrhea, or both for more than 6 hours.
- You’ve vomited every time you ate something in the past 24 hours.
- You don’t think you can take care of yourself and don’t have anyone to help you.
You may take one of these medicines:
- Metformin (Glucophage®).
-
An SGLT-2 inhibitor medicine. Examples include:
- Invokana®
- Jardiance®
- Farxiga®
- Steglatro®.
- A medicine that has metformin or an SGLT-2 inhibitor in it.
Call your healthcare provider if you take one of the medicines listed above and:
- You have vomiting, diarrhea, or both that won’t stop.
- You’re eating and drinking much less than usual.
- You’re scheduled for any type of surgery.
- You have an infection.
- You’re taking much less insulin than usual.
If you’re a patient at MSK and you need to reach a healthcare provider after , during the weekend, or a holiday, call 212-639-2000.
When to go to the emergency room
Call your healthcare provider and go to the emergency room if:
- You cannot stay awake or think clearly. If this happens, someone should take you to the emergency room and call your healthcare provider for you.
- Your blood glucose goes below 70 mg/dL and you cannot eat or drink to raise it to a normal level.
-
You have any signs of DKA, such as:
- Fruity-smelling breath
- Fast breathing or trouble breathing.
- Abdominal (belly) pain.
- Feeling confused.
- Moderate to high ketone levels in your urine.
Follow-up care
Within 1 week after discharge
It’s important to share your blood glucose readings with your outpatient diabetes healthcare provider within 7 days after you’re discharged. You may need to talk to them sooner if:
- You were just diagnosed with diabetes or hyperglycemia.
- You were discharged with a feeding tube.
- You’re tapering off steroids.
- You’re trying to get your blood glucose to a target range to continue treatment.
- Your medicine regimen (the medicines you take) has changed.
- Your blood glucose levels are not within your target range.
Some of your healthcare providers often do not manage blood glucose levels or adjust diabetes medicine. This can include your oncologist (cancer doctor), surgery team, or radiation oncologist.
Follow up with your primary healthcare provider or diabetes healthcare provider to manage your blood glucose levels after you’re discharged. If you do not have a primary healthcare provider or endocrinologist, tell a member of your care team. They can help set up follow-up care.
Routine follow-up
Certain appointments and testing are part of routine care for people with diabetes. These are how we check for problems caused by diabetes early, when they’re easier to treat.
Your endocrinologist will help make a care plan that is right for you. They will usually check your hemoglobin (HEE-moh-GLOH-bin) A1c (HbA1c) levels every 3 months. HbA1c is the measure of your average blood sugar level over the past 3 months.
Write in your diabetes providers information here:
- Name: ____________________________________
- Phone number: ____________________________________
- Email: ____________________________________
- Fax: ____________________________________
- Next appointment: ____________________________________
Educational resources
This section lists the MSK educational resources mentioned in this guide. Always read the written version even if you watch the video. There’s important information in the written version that may not be in the video.
- About Newly Diagnosed Type 1 Diabetes Mellitus (T1DM)
- How to Check Your Blood Glucose (Blood Sugar) Using a Blood Glucose Meter
- Contour® Next One Video: Doing Your First Test
- About Hyperglycemia (High Blood Sugar)
- About Hypoglycemia (Low Blood Sugar)
- About Insulin for Diabetes or Treatment-Related Hyperglycemia
- How To Manage Your Blood Glucose (Blood Sugar) With Your Diet
- About Emergency Glucagon Treatments
- Diabetic Ketoacidosis (DKA) and Ketone Urine Testing
- How to Manage Diabetes When You’re Sick
More diabetes resources
American Diabetes Association
www.diabetes.org
Breakthrough T1D
www.breakthrought1d.org
Calorie King
Visit www.calorieking.com or download the smartphone app.
My Fitness Pal
Visit www.myfitnesspal.com or smartphone app.
