In January, the American Cancer Society reported that the rate of cancer deaths in the United States had fallen 2.2% from 2016 to 2017. This was the largest single-year decline in cancer mortality ever reported.
Many factors have contributed to the continuing decline in cancer deaths. The reduction in the number of people who smoke is chief among them. But advances in diagnosis and treatment, especially those made during the past ten years, have also played a significant role. Experts anticipate that, with further advances in research, cancer survival will continue to improve over the next decade and beyond.
In an interview, Larry Norton, a medical oncologist and Senior Vice President at Memorial Sloan Kettering, talked about some of the biggest achievements in cancer care made between 2010 and 2019, and what he hopes to see next.
Immunotherapy
By any estimate, immunotherapy has been the past decade’s most noteworthy advance in cancer medicine. It was one of the earliest attempts regarding the nonsurgical treatment of cancer. Making it effective, though, has taken more than 100 years, coming into its own only in the 2010s.
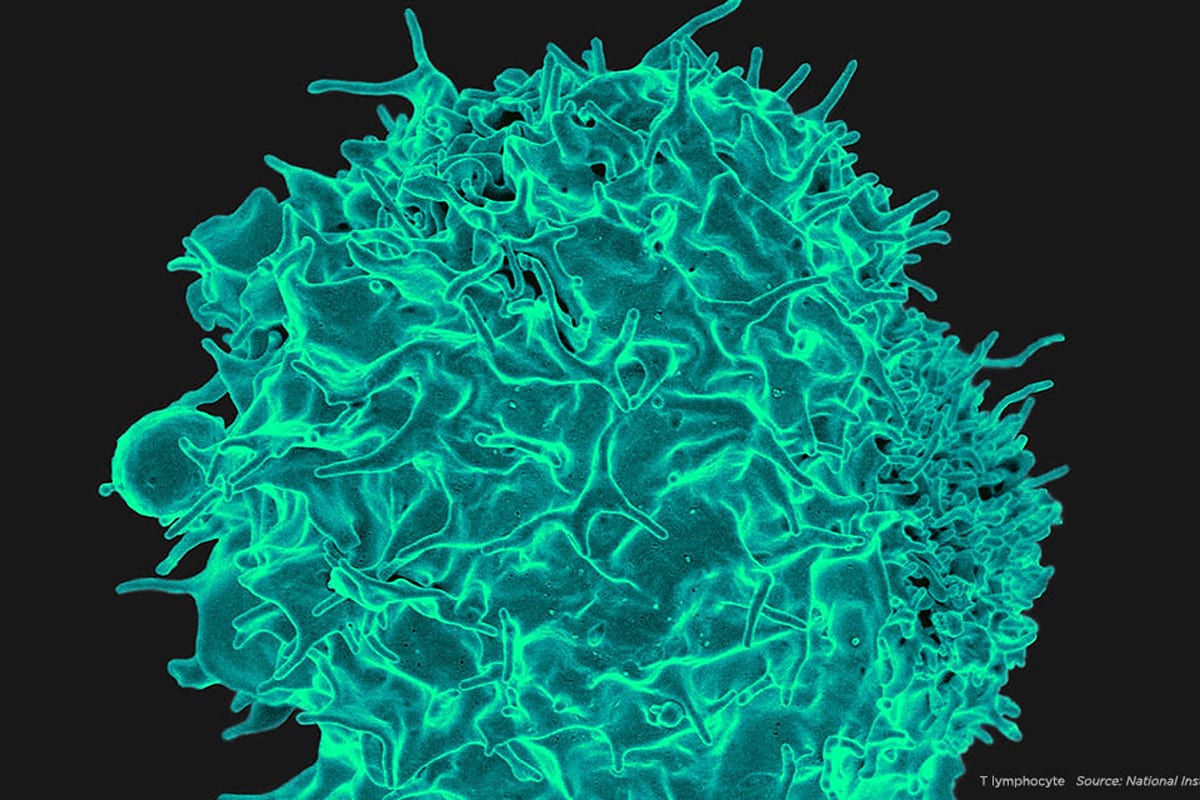
At Memorial Sloan Kettering, we believe that immunotherapy is one of the most promising ways to treat, cure, and ultimately prevent cancer.
The field dramatically accelerated in 2011 with the US Food and Drug Administration’s approval of ipilimumab (Yervoy®) for melanoma. This drug, in a class called immune checkpoint inhibitors, was based on research conducted by immunologist James Allison and developed in clinical trials with the help of MSK physician-scientists. Dr. Allison, who led the Sloan Kettering Institute’s Immunology Program from 2002 to 2012, won a Nobel Prize in 2018 for this pioneering work. Several other checkpoint inhibitor drugs followed. What these therapies have in common is that they take the brakes off the immune system, enabling it to destroy cancer.
“In addition to melanoma, these are some of the first new drugs to really have an impact on lung cancer,” Dr. Norton says. “They also have become very important for treating bladder cancer and other cancers.”
Chimeric antigen receptor (CAR) T cell therapy was another big leap forward in immunotherapy. In this approach, pioneered by MSK’s Michel Sadelain, scientists genetically engineer a patient’s own immune cells to make a new protein that can latch on to cancer. This turns those altered cells into powerful cancer fighters.
What’s Next?
Researchers are looking for ways to make immunotherapy drugs effective in more people and for more types of cancer. One approach that’s promising is using cancer vaccines and viruses to activate tumor cells and make them more visible to the immune system. These treatments are likely to be combined with checkpoint drugs and CAR T.
Targeted Therapies
Targeted therapies came into their own in the late 1990s and early 2000s, with the approval of drugs like trastuzumab (Herceptin®) and imatinib (Gleevec®). But in the 2010s, they became part of standard treatment for many more cancers. Dozens of new drugs were approved for both solid tumors and blood cancers. These therapies are designed to exploit weaknesses found primarily in cancer cells while sparing healthy tissue.
Thanks to studies called basket trials, researchers have learned that the same drug may work against many types of cancer if the tumors have the same genetic changes. One of the most striking examples of this pan-cancer approach is larotrectinib (Vitrakvi®), which the FDA approved in 2018.
Advances in targeted therapy for blood cancers, especially chronic lymphocytic leukemia, acute myeloid leukemia, and acute lymphocytic leukemia, have led to a number of drug approvals. These drugs have fewer side effects than traditional chemotherapy. Because of that, they can be given to people who are unable to tolerate more intense treatment because of their age or other health problems.
What’s Next?
Researchers are learning more about how tumors develop resistance to targeted drugs. In addition, they’re studying the role of tumor heterogeneity, which allows some tumor cells to escape the effect of these drugs.
According to Dr. Norton, another exciting area of research is tackling the noncancerous cells that surround tumors, called the tumor microenvironment. “Some of these cells stimulate cancer growth, and we can also go after them with drugs,” he says. “To paraphrase a Zen koan: Targeting only the tumor is like trying to clap with one hand. You may have to hit both sides of the equation to really make a difference.”
Molecular Diagnostics
With the development of tests like MSK-IMPACT™, launched in 2014, and MSK-ACCESS, launched in 2019, doctors now have the ability to look for hundreds of cancer-causing mutations across of range of tumor types with a single test. As of the end of January 2020, more than 50,000 tumors from more than 43,000 patients have been analyzed with MSK-IMPACT. More recently, MSK-ACCESS has enabled doctors to study tumors using a blood test called a liquid biopsy rather than having to do a more complicated tissue biopsy.

What’s Next?
Molecular diagnostics looks for a number of changes in cells. These might include chromosomal gains and losses, changes in gene copy numbers, structural rearrangements, and broader mutational signatures. Analysis of messenger RNA (the genetic material that carries information from DNA to a cell’s protein-making machinery) is becoming an important diagnostic tool, too.
Unlike other genetic tests, MSK-IMPACT and MSK-ACCESS look for mutations in a person’s normal tissue for comparison. This bonus analysis is revealing new clues about which cancers are inherited.
Diagnostic tests that include normal tissue are also uncovering more details about clonal hematopoiesis (CH). This age-related condition leads to an increased number of white blood cells that carry cancer-causing mutations. CH is not cancer, but people who have it have an increased risk of cancer. “We’re learning more and more about the role that CH cells play in relation to many kinds of cancer, not just blood cancers,” Dr. Norton says.
Screening and Early Detection
In the 2010s, large studies confirmed the benefits of many screening tests, such as colonoscopies for colon and rectal cancer and low-dose CT scans for people at an increased risk of lung cancer because of their smoking history. There have been a number of advances in mammograms and other types of breast screening as well. For example, MRIs can be used to classify a woman’s risk of developing breast cancer.
What’s Next?
Dr. Norton says that the personalization of cancer screening will play a big role over the next decade. “Not everyone needs to have the same level of monitoring,” he notes.

MSK’s Precision Interception and Prevention program combines the principles of precision medicine with research on prevention and early detection. The goal of this approach is to prevent cancer from occurring or stop it at the earliest stages, when it’s easier to treat.
Surgery
Over the past ten years, minimally invasive and robotic surgeries have become standard for more and more cancers. For many cancer types, studies have confirmed that these surgeries are just as effective as open surgeries at controlling disease but with less pain and quicker recovery.
“Many of these surgical techniques have been advanced at MSK’s Josie Robertson Surgery Center,” Dr. Norton says. The center, which opened in 2016, enables surgeons to perform outpatient procedures in a state-of-the-art setting. More than half of the 20,000 surgeries done at MSK every year are now done on an outpatient basis.
What’s Next?
Although surgery will continue to be an important part of cancer care, Dr. Norton says that continuing advances in other treatments will enable some people to avoid surgery entirely. “For some people with breast cancer, drug therapies and radiation are becoming so effective that we might want to do research looking at whether they might not need surgery or will need only minimally invasive surgery,” he says.
Radiation Therapy
In radiation therapy, one of the important tenets over the past decade has been “less is more.” Advances like intensity-modulated radiation therapy and image-guided radiation therapy use computer programs and advanced imaging to deliver stronger doses of radiation while sparing healthy tissue. Oftentimes, fewer radiation treatments are needed to achieve the same benefits. There have also been advances in identifying which tumors can be effectively controlled with less radiation overall, which reduces side effects.
What’s Next?
In 2019, the New York Proton Center opened in East Harlem. The center aims to provide treatment and to conduct clinical trials comparing proton therapy to other types of radiation. Proton therapy is already in use, especially for head and neck cancers and pediatric tumors. Experts expect it to become more widely used in the 2020s.
Pediatric Cancer
Survivorship rates for pediatric cancers continued to improve in the 2010s. About 80% of children with cancer can now be cured with available treatments. For the remaining 20%, there has been an increased focus on personalized medicine.
All children treated at MSK Kids receive testing with MSK-IMPACT. And clinical trials developed by MSK’s Early Drug Development Service can now include children as young as 12. For children with very rare mutations, protocols for single-patient use (SPU) can provide lifesaving treatment.

What’s Next?
Initiatives like MSK’s Pediatric Translational Medicine Program and the Expanded Genomics Program aim to make personalized medicine an option for more children with cancer. And when investigators conduct SPUs, they collect data to learn how and why certain drugs work or don’t. These findings can lead to future trials.
Supportive Care and the Patient Experience
Research reported in 2017 confirmed that systematic monitoring of patient-reported symptoms during chemotherapy improves survival outcomes. Patient input and the patient experience are now incorporated into the design of clinical trials. These measures empower patients to actively report their symptoms. Doctors and nurses are then able to intervene early, ultimately improving patients’ quality of life as well as survival rates.
What’s Next?
Investigators at MSK are continuing to focus on the influence of nutrition, integrative medicine, and exercise in improving patients’ well-being during and after treatment — as well as their cancer outcomes. Digital health and telemedicine are another exciting frontier in cancer management and research, Dr. Norton says. Clinical trials already underway aim to look for measurable benefits from these interventions.
Many of the advances in cancer treatment and diagnosis seen over the past ten years are possible thanks to funding from donors, Dr. Norton explains. “You can make progress with philanthropic support that you can’t accomplish any other way,” he says. “It gives researchers freedom to be creative in a way that no other type of funding makes possible.”