本資訊將幫助您作好準備,以便在 MSK 接受乳房或胸壁體外放射治療。 這將幫助您了解在接受放射治療前後和期間的預期情況,以及如何照護自己。
關於放射治療
放射治療使用高能量射線來治療癌症。 這些射線可以損壞癌細胞,令其難以繁殖。 然後,您的身體便能代謝掉受損的癌細胞。 放射治療也會影響正常細胞,但它們可以利用一種癌細胞無法做到的方式自我修復。
放射治療需要一定的時間才會見效。 接受治療數天甚至數星期後,癌細胞才會開始死亡。 在放射治療結束後的幾星期或幾個月內,這些細胞會持續死亡。
在 MSK,大多數人會在手術後接受乳房或胸壁放射治療。 如您的治療計劃包括化療,則您可能會在完成化療後 4 星期開始放射治療。 我們會與您討論相關的預期情況。
關於體外放射治療
體外放射治療是一種放射治療。 在體外放射治療中,治療機器將由您的體外對目標區域照射一束射線。 射線會穿過您的身體,破壞沿途的癌細胞。 您不會見到或感受到射線。
您可能有以下一個或多個部位正在接受放射治療:
- 胸部。
- 胸壁。
- 頸骨旁的淋巴結。
- 腋下的淋巴結。
- 胸骨附近的淋巴結。
您的放射腫瘤醫生和護士將與您討論相關治療計劃。
您在放射治療團隊中擔當的職責
您的放射治療照護團隊將共同合作為您提供醫療照護。 您也是這個團隊中的一個成員,而您在當中的職責包括:
- 準時應診。
- 提問並說出您的憂慮。
- 出現副作用時告知我們。
- 感到疼痛時告知我們。
-
透過以下方式在家中照護自己:
- 如有吸煙,應戒煙。 MSK 有專家可以幫助您。 如欲更深入了解我們的戒煙計劃,請致電 212-610-0507。 您也可以向護士查詢該計劃的詳情。
- 根據我們的指示來護理皮膚。
- 根據我們的指示來飲用液體。
- 食用或避免食用我們建議的食物和飲品。
- 保持大致相同的體重。
乳房或胸壁放射治療前
模擬治療
在開始放射治療前,您將進行一項稱為模擬治療的治療計劃程序。 在模擬治療期間,您不會接受任何放射治療。
在模擬治療期間,您的放射治療師將進行成像掃描。 他們可能會用細小的紋身點來標記皮膚。 這將有助我們:
- 測繪受治療部位。
- 確保您獲取劑量合適的放射射線。
- 限制進入治療部位附近組織的放射射線。
您的模擬治療將需時 60 至 90 分鐘。
止痛藥
在模擬期間,您將會保持一個姿勢約 30 至 60 分鐘。 確切的時間長短取決於您的放射治療計劃。 如果您認為長時間靜止不動會不舒服,請告訴我們。 您也可以在預約前的 1 小時服用非處方止痛藥或常用的止痛藥。
衣著
請穿著舒適且容易脫下的服裝。 您將需要脫下上身衣物並換上醫院的長外衣。
除非照護團隊成員告訴您可以,否則不要佩戴珠寶,不要塗粉或使用任何乳液或面霜。
取下皮膚上的裝置
您的皮膚上可能佩戴有特定裝置。 一些裝置製造商建議您在模擬治療或治療前取下:
- 連續血糖監測儀 (CGM)
- 胰島素泵
如果您使用其中一種裝置,請諮詢您的放射腫瘤醫生是否需要取下。 如需取下裝置,請確保您有攜帶後備的裝置 ,供您在模擬治療或治療後穿戴。
您可能不確定在裝置關閉時該如何管理血糖。 如果是這樣,在您預約之前,請向為您管理糖尿病事宜的保健提供者諮詢。
到達後的預期情況
當您到達後,放射治療團隊成員會為您辦入院手續。 他們會為您提供一條附有姓名和出生日期的身份識別 (ID) 手環。 預約期間,許多工作人員會檢查您的 ID 手環,並要求您說出並拼寫自己的姓名和出生日期。 這是出於您的安全考慮。 可能有姓名相同或相似的人在同一天接受照護。
放射治療師將審查模擬治療期間的預期情況。 如果您尚未簽署同意書,他們將與您一同審視其內容。 他們會解答所有疑問,並請您簽名確認。
模擬治療期間
您將需要脫下上身衣物並換上醫院的長外衣以進行模擬治療。 醫務人員將帶您前往更衣室。 不要脫下鞋子。 如您需要幫忙換衣服,請告訴放射治療團隊成員。 照護提供者將在更衣室裡幫助您。
如果您有佩戴頭飾,可能需要先將其取下。 頭飾的例子包括假髮、頭巾和帽子。
當您準備好時,治療師會帶您去模擬室。 他們會幫助您躺在治療床上。 床上有鋪床單,但質地仍然很硬,而且沒有墊子。 如您尚未服用止痛藥,且認為自己可能有此需要,則請告訴放射治療師。 如果可以,請在模擬開始前告訴他們。
在整個模擬治療期間,您會感到治療床移至不同的位置。 放射治療師將打開和關閉房裡的燈。 您將在每面牆上看到紅色或綠色雷射光線。 您的放射治療師為您在床上定位時,會以這些雷射光線作為指引。 請不要直視雷射光線。 雷射光線可能會損害眼睛。
您的放射治療師會在您的模擬治療過程期間進出房間。 始終會有人看到您並能聽到您說話。 您會聽到放射治療師一邊工作一邊交談。 他們亦會向您講解他們正在做甚麼。
此外,模擬室通常溫度較低。 如您感到不適,請隨時告知放射治療師。 他們將盡一切努力確保您舒適並享有隱私。
定位
您可以仰躺或俯躺。 不論是何種姿勢,您的一隻或兩隻手臂都將舉起至高過頭部。 模擬治療一旦開始,請勿移動。 保持同一姿勢非常重要。 如果您感到不適或需要協助,請告訴您的放射治療師。
深呼吸保持 (DIBH)
在進行模擬治療和治療時,放射治療師可能會要求您每次屏住呼吸 15 至 20 秒。 是否這樣要求取決於您的治療計劃和體形。 照護團隊會告訴您是否需要這樣做。
若要了解更多,請觀看About Deep Inspiration Breath Hold (DIBH) and the Visual Coaching Device。
成像掃描
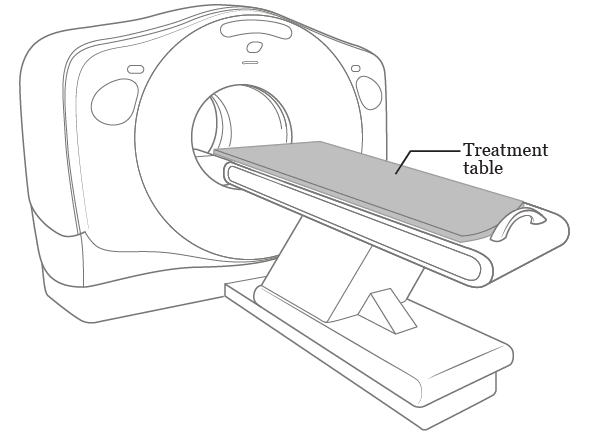
受治療部位將接受成像掃描。 這些掃描可能會以名為「模擬器」的 X 光機進行,也可能會以電腦斷層掃描 (CT) 掃描機進行(見圖 1)。 我們將使用這些掃描來制定您的治療計劃。 我們不會將其用於診斷或找尋腫瘤。 如您需要進行其他成像掃描,則放射護士將告訴您預期的情況。
成像掃描大約需要 45 分鐘。 在掃描期間,您會聽到機器開啟和關閉。 雖然噪音似乎很大,但如果您向放射治療師說話,他們還是能夠聽到您的聲音的。
皮膚標記(紋身)
放射治療師或會使用氈頭筆在治療區域的皮膚上作標記。 您可能還需要稱為紋身的皮膚標記。 並非每個人都需要紋身。 照護團隊會與您討論相關的預期情況。
如您需要紋身,放射治療師會使用殺菌(清潔)針頭和一滴墨水進行繪製。 每個紋身都會感到被針刺扎。 它們不會超出針頭大小。
紋身完成後,放射治療師將會為您的治療位置拍攝照片。 他們將使用這些照片和紋身來確保您在接受放射治療時處於正確的位置。
模擬後,氈頭筆的標記可以洗掉。 如您需要紋身,它們是永久的。 無法洗掉。 如果您對於接受放射治療時需要紋身感到憂慮,請向您的放射腫瘤醫生諮詢。
安排放射治療
在模擬治療的預約結束時,您將就設置程序和放射治療預約作出安排。 您還將獲分配至一部放射治療儀器進行放射治療。
您的放射腫瘤醫生將與您討論相關治療日程。
- 接受腫瘤切除手術後,醫生會在您接受放射治療時與您討論是否需要全乳腺或部分乳腺放射治療。 大多數人每天接受放射治療,持續 1 到 4 星期。
- 如您接受放射治療的位置是胸壁或鎖骨附近的淋巴結、腋下或胸骨附近的淋巴結,您將每天進行放射治療,持續 5 至 6 星期。
您必須接受每一次放射治療。 如您錯過治療,則放射治療可能不會有那麼好的效果。 如您因任何原因無法接受某次治療,請致電放射腫瘤醫生的辦公室以通知放射治療團隊。 如您因任何理由而需改期,請向您的放射治療師諮詢。
治療規劃
在完成模擬治療後和首次治療開始前,您的放射腫瘤醫生會與團隊合作,規劃您的治療。 他們將使用模擬過程期間進行的成像掃描來規劃射線的角度和形狀。 他們將精心計劃並檢查細節。 此過程需時 1 至 2 星期。
乳房或胸壁放射治療期間
放射治療期間的維他命及膳食補充劑
放射治療期間可以服用複合維他命。 任何維他命或礦物質都請勿攝取超出所建議的每日上限 (RDA)。
在未與照護團隊成員商討的情況下,請勿服用其他膳食補充劑。 維他命、礦物質和草本或植物(植物基)補充劑都是膳食補充劑的例子。
避免抗氧化劑補充劑,例如:
|
|
您不需要從飲食中去除這些抗氧化劑。 如您想與臨床營養師討論您的飲食或補充劑,請告訴您的放射護士。
皮膚照護
在您首次接受放射治療的當天,您將開始在受治療部位塗抹去炎松 0.1% 軟膏。 這是可以幫助保護皮膚的處方軟膏。 您將每天使用此藥膏,早晚各一次。 包括您沒有接受治療的日子。 放射護士會在首次治療前為您提供更多這方面的資訊。
放射腫瘤醫生也可能會建議在受治療部位使用 Mepitel® 保薄膜來保護您的皮膚。 如有需要,護士將在首次治療前在受治療部位上使用 Mepitel 保護膜。 請一直敷着直到其邊緣開始脫落。 如果邊緣開始脫落,請視需要向放射護士尋求修補或更換。
放射治療預約
因應治療計劃,您在每次放射治療期間將保持同一姿勢約 10 到 20 分鐘。 如果您認為自己躺太久會不舒服,可以在應診前 1 小時服用對乙醯氨基酚 (Tylenol) 或常用的止痛藥。
設置程序
在首次接受放射治療時,您將進行一個設置程序。 設置程序及首次治療通常需時約 1 小時。
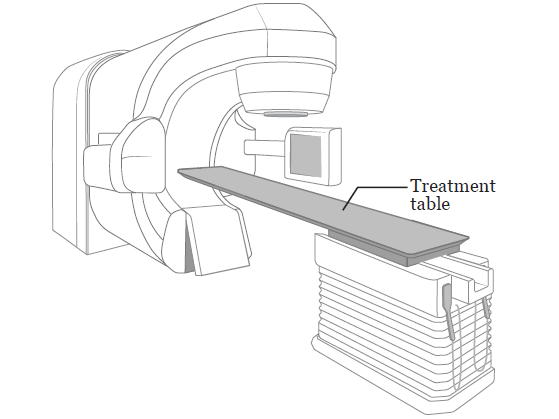
每天,放射治療師會帶您到接受放射治療的房間。 他們將幫助您在治療桌上躺下(請參見圖 2),姿勢與模擬治療期間的姿勢相同。
放射治療師將拍攝特殊的 X 光照片(稱為束膜),以確保您的姿勢和受治療部位正確。 束膜會在您治療期間不斷重覆。 束膜並不會用來審視您對治療有何反應。
放射治療期間
在治療期間,您會處於與模擬和設置程序時完全相同的位置。 放射治療師將盡一切可能確保您感到舒適。 您以正確姿勢就位後,放射治療師便會離開房間,關上房門,然後開始為您治療。
在接受放射治療時請保持靜止。 您不會看到或感受到輻射,但機器在您身邊移動和開關時,您可能會聽到機件聲音。 在整個治療過程中,放射治療師都能透過監視器看到您,並且可以利用對講機與您交談。 如您感到不適或需要協助,請告訴他們。
您會在治療室逗留 10 至 20 分鐘,實際需時取決於您的治療計劃。 您將花費大部分時間來確保自己處於正確的位置。 實際治療只需數分鐘。
放射治療不會使您免疫力下降(削弱免疫系統)。 放射治療不像化療那樣會影響血球計數。
放射治療不會使您或您的衣服具有放射性。 即使您與他人一起也是安全的。
關於加強治療
您可能會在完成放射治療的第一部分後獲得一次額外的輻射劑量(稱為加強治療)。 在加強治療期間,射線會專注於發現腫塊或癌細胞的區域, 而不會射向整個乳房。 照護團隊將告訴您是否需要進行加強治療。
加強治療預約期間
在進行加強治療前,您的放射治療師將使用氈頭筆在皮膚上作標記,勾勒出接受加強治療的部位。 穿一件您不介意弄髒的衣服。 氈頭筆的染料可能會弄髒您的衣服。 此外,這些皮膚標記並不是永久的。 在完成治療前,請勿將它們擦掉。
您將接受的射線劑量與其他治療大致相同,但將針對更小的區域進行照射。 對於加強治療,您可能會使用不同的治療機器或躺在不同的位置。
狀態檢查訪視
放射腫瘤醫生和護士將每星期與您見面,討論您的憂慮,詢問您有否出現任何副作用,並回答您的問題。 在這些日子,請預計應診時間需要多花大約 15 到 30 分鐘。
在這些訪視期間,放射腫瘤醫生和護士將檢查受治療部位的皮膚狀況。 他們或會開立軟膏、霜劑或特殊敷料來護理您的皮膚。
如您需要在狀態檢查視訪之間與放射腫瘤醫生或護士交談,請致電放射腫瘤醫生的辦公室。 您也可以請輻射治療師或其他工作人員與他們聯絡。
每週電郵
我們每星期也會透過電郵傳送一份症狀相關的問卷給您。 這份問卷有助放射治療團隊了解您的狀況,以及有否出現任何副作用。 在完成放射治療後的 6 星期內,您每星期將填寫一次問卷。
閱讀Communicating With Your Care Team: When to Call or Use MSK MyChart及How to Take Pictures of Your Skin for Your Healthcare Provider將對您有所幫助。
乳房或胸壁放射治療的副作用
放射治療可能會帶來一些副作用。 這些副作用的類型和強度取決於許多因素。 這些因素包括射線劑量、治療次數以及整體健康狀況。 如您同時接受化療,則副作用可能會更嚴重。
在放射治療開始的約 2 至 3 星期後,您可能會開始注意到副作用。 這些副作用可能會在接受放射治療後的 1 至 2 星期內加重,但在最後一次治療後的 4 至 6 星期內會逐漸改善。 有些副作用可能需要更長的時間才會消失。
請遵循本節中的指南,以幫助管理在接受放射治療期間和之後出現的副作用。
皮膚和毛髮反應
在接受放射治療期間,受治療部位的皮膚和頭髮會出現變化。 這是正常情況。
- 您的皮膚可能會變成粉紅色、紅色、古銅色或看起來像被曬傷。 腋下和乳房的皮膚皺褶、鎖骨上方以及其他暴露於陽光下的受治療部位皮膚可能會起水泡和脫皮。
- 您的皮膚可能會變得非常敏感和發癢。
- 您可能會出現皮疹,尤其是在暴露於陽光下的皮膚。如果在放射治療期間出現皮疹,請隨時告知放射治療團隊成員。 皮疹有時是感染的徵兆。
- 在接受治療一側的腋下,您可能會失去部分或全部毛髮。 通常會在您完成放射治療後的 2 至 4 個月內重新長出來。
如果您的皮膚裂開、濕潤和有液體滲出,請聯絡放射治療團隊。 他們可能會開立名為 Silvadene®(磺胺嘧啶銀)的藥膏。 放射腫瘤醫生可能會暫停放射治療,直到您的皮膚癒合為止。 大多數人不需要中止治療。
放射治療引起的皮膚反應通常在完成放射治療後的 1 到 2 星期內最為嚴重,然後開始愈合。 通常需要 3 到 4 星期才能愈合。 如有任何問題或疑慮,請立即聯絡放射腫瘤學醫生或護士。
皮膚照護指南
在治療期間,請遵循這些指南來護理皮膚。 請一直遵循這些指南,直至您的皮膚有所改善。 這些指南僅適用於受治療部位的皮膚。
放射護士會在首次治療前為您提供更多護理皮膚的資訊。 可能包括使用軟膏、霜劑、特殊敷料,或者三者兼用。 請遵循他們的指引。
- 每天利用溫水和溫和無香料皂(如 Neutrogena®、Dove®、嬰兒皂、Basis® 或 Cetaphil®)泡澡或淋浴。 徹底沖洗皮膚,然後以柔軟的毛巾拍乾。
- 您可在受治療部位的未破損皮膚上使用止汗劑。 如果出現皮膚敏感,請即停止使用。
- 清洗時,應溫柔對待受治療部位的皮膚。 不要為皮膚去角質。
- 您在治療前紋在身上的標記會永久存在,無法洗掉。 您可能會在治療期間以紫色氈頭筆標上其他標記,例如治療部位的外形輪廓。 得到放射治療師同意後,您便可以用礦物油移除這些標記。
- 每天在受治療部位塗抹一層去炎松 0.1% 軟膏 2 次。 如您只是薄塗一層軟膏,則在接受放射治療前不需要將其擦掉。 在放射治療結束後的兩星期,請持續每天使用去炎松 0.1% 軟膏 2 次。
- 請勿在受治療部位的皮膚上使用酒精或酒精棉片。
避免刺激受治療部位的皮膚
- 受治療部位應穿著鬆身的棉質衣物和內衣。 請避免穿著會磨擦皮膚的緊身衣物(包括有鋼圈的胸圍)。
- 請勿在受治療部位的皮膚上使用化妝品、香水、粉餅或鬚後水。
- 請勿將膠貼貼在受治療部位的皮膚上。 包括帶有黏力的繃帶。
- 如果皮膚發癢,請勿抓撓。 每天塗抹去炎松 0.1% 軟膏 2 次。 這是最佳的止癢治療。
- 避免在受治療部位除毛。 如果必須剃除,請僅使用電動鬚刨。 如果出現皮膚敏感,請即停止。
- 請勿讓受治療皮膚接觸到極端的高溫或低溫。 包括熱水浴缸、水樽、電熱毯和冰袋。
- 如果您在治療期間沒有皮膚反應,可以在已氯化消毒的泳池中游泳。 在離開泳池後立即沖掉氯。
- 治療期間和往後的生活中,請避免曬黑或曬傷皮膚。 如果您將受到太陽照射,請使用防曬係數 (SPF) 達 30 或以上的防曬霜。 應穿著可盡量遮蓋所有皮膚的鬆身衣物。
乳房不適或腫脹
在受影響一側的乳房,尤其是在乳頭附近,您可能會感到些許壓痛。 您的乳房中可能會積聚多餘液體,因而引起劇烈刺痛感。 您的乳房或胸部可能會感到沉重或腫脹。 受影響一側的肩膀可能也會變得僵硬。
這些感覺可能會在您接受放射治療的最初幾天內開始出現。 在您完成放射治療後,這些感覺可能會持續數月。 以下是幫助您減輕這種不適的建議。
- 如果您穿胸圍,則可能會選擇柔軟、寬鬆的無鋼圈胸圍。 運動型或棉質胸圍是不錯的選擇。 您甚至可能會發現完全不穿胸圍更舒適。
- 根據需要服用止痛藥,例如非甾體抗炎藥 (NSAID)。 NSAID 的一些例子包括布洛芬 (Advil®) 和萘普生 (Aleve®)。 如您不能服用 NSAID,則可以選擇服用乙醯胺酚 (Tylenol) 替代。
疲勞
疲勞會令人感到疲倦或虛弱、無心做事、無法集中,或是感到行動變慢和缺乏能量。
您可能會在接受放射治療 2 至 3 星期後開始出現疲勞症狀。 疲勞程度可能從輕微到嚴重不等,且在某些時間可能會更為嚴重。 疲勞在您完成放射治療後會逐漸消失,但可能會持續數月。
控制疲勞
- 如果您有在工作,而且並沒有覺得不適,那麼繼續工作是可以的。 如果您感到疲勞,則減少工作可能有助增加精力。
- 規劃您的日常活動。 選擇需要或真正想做的事情,並在精力最好的時候去完成這些事。 例如,您也許可以去上班但不做家務,或是去觀看孩子的體育活動但不外出吃晚餐。
-
每天規劃一些時間來休息或小睡片刻(10 至 15 分鐘),尤其是當您感到特別疲倦時。
- 每天晚上儘量保證 8 小時睡眠。 這也許會比您開始放射治療前所需的睡眠時間更長。 此外,您也許會發現以下做法有所幫助:
- 早睡晚起。
-
在白天保持活動。 例如,如果您能做運動,可以外出散步、做瑜伽或踏單車。
- 睡前放鬆身心。 例如,看書、玩砌圖、聽音樂,或做一些令人平靜下來的興趣活動。
- 請家人和朋友協助您處理家務和跑腿。 請向您的保險公司查詢,看看他們的保單服務有否涵蓋家居照護服務。
- 某些人做運動會更加精力充沛。 請向放射腫瘤醫生諮詢您能否做輕量運動,例如散步、拉伸或瑜伽。 請參閱Managing Cancer-Related Fatigue with Exercise,以了解更多資訊。
- 進食和飲用含有豐富蛋白質和高卡路里的食物和飲料。 請閱讀癌症治療期間的良好飲食或Nutrition and Breast Cancer: Making Healthy Diet Decisions,以了解更多資訊。
疼痛、噁心(想吐)、腹瀉(稀薄或水狀的排便)、失眠、抑鬱或焦慮等症狀可能會加重疲勞症狀。 請就您可能出現的任何其他症狀向放射腫瘤醫生或護士求助。
性醫學及生殖醫學健康
除非放射腫瘤醫生另有指示,否則您可以在接受放射治療期間進行性行為。 您不會具有放射性,也不會將輻射傳給他人。 如果您或性行為對象有懷孕的可能,則在接受放射治療期間使用避孕措施很重要。
您也許會擔心癌症和您的治療會對性生活有何影響。 您身上並無輻射。 您不會將輻射傳給他人。 即使與他人密切接觸也很安全。
除非放射腫瘤醫生另有指示,否則您可以在接受放射治療期間進行性行為。 如果您或您的伴侶有生育能力,您便應該避孕,以防在放射治療期間懷孕。
與放射腫瘤醫生或護士討論性健康可能很難,但這是一個需要討論的重要話題。 除非您分享自身的問題和憂慮,否則他們可能不會提及。 您可能會感到不自在,但大多數接受癌症治療的患者都有類似問題。 我們努力確保我們照護的每個人都覺得自己獲接納。
性健康計劃
MSK 提供性健康計劃。 這些計劃能助您管理癌症或其治療對您的性健康或生育能力所帶來的影響。 我們的專家可以助您在放射治療前後或期間處理性健康或生育問題。
- 如需更多有關女性性醫學及女性健康計劃的資訊,或想作出預約,請致電 646-888-5076。
- 如需更多有關男性性醫學及生殖醫學計劃的資訊,或想作出預約,請致電 646-888-6024。
- 如要了解與我們的癌症與生育計劃相關的資訊,請與您的保健提供者交談。
其他性健康資源
閱讀Sex and Your Cancer Treatment,了解更多有關癌症治療期間性健康的資訊。
美國癌症學會亦設有關於癌症治療期間性行為方面的資源。 分別是性與成年男性癌症患者和性與成年女性癌症患者。 您可以到 www.cancer.org 找到此等資源,或是致電 800-227-2345 索取影印本。
情緒健康
|
|
|
您也許會擔心要告知僱主您患上癌症,或是因醫療費用而擔憂。 您可能會擔心家人關係出現轉變,或癌症會復發。 您可能會擔心癌症治療對您身體造成的影響,或者擔心自己是否會失去魅力。
這些擔心均屬正常,並且是可以接受的。 當您或所愛之人患上嚴重疾病,出現上述感受是正常反應。 我們會為您提供協助。
處理情感的方式
與他人傾談。 當人們為了保護彼此而隱藏自身感受,他們可能會感到非常孤單。 傾談有助您身邊的人瞭解您的想法。 和您信任的人討論您的感受,可能會有所幫助。 例如,您的傾談對象可以是伴侶或配偶、好朋友或家人。 您也可以與牧師(精神顧問)、護士、社工或是心理學家交談。
加入支援小組。 和其他癌症患者見面,可讓您有機會談及自己的感受,以及從他人身上學習。 您會得知其他人如何面對癌症和治療,同時提醒您並非孤軍作戰。
我們知道每個癌症診斷和每個癌症患者都不盡相同。 我們為那些診斷或身份相似的人士提供支援小組。 例如,您可以加入乳腺癌患者或 LGBTQ+ 癌症患者的支援小組。 請瀏覽 www.msk.org/vp,了解更多關於 MSK 支援小組的資訊。 您也可以與放射腫瘤醫生、護士或社工交談。
嘗試放鬆和冥想。 這類活動有助您感到放鬆和冷靜。 您可以試著想象自己身處最喜歡的地方。 與此同時,慢慢呼吸。 專注於每一次呼吸,或聆聽舒緩的音樂或聲音。 對某些人來說,祈禱是另一種形式的冥想。 請瀏覽 www.msk.org/meditations,找到由我們綜合醫學與健康服務提供者引導的冥想指導。
做運動。 很多人發現,散步、踏單車、瑜伽或水中有氧運動等輕量運動有助他們感覺好過一點。 請向您的保健提供者查詢您可以做甚麼類型的運動。
每個人都有其處理困境的方式。 通常,我們會使用以往對我們自己有效的方法。 但是,有時候這樣並不足夠。 我們鼓勵您積極與您的醫生、護士或社工談及您的憂慮。
乳房或胸壁放射治療後
覆診預約
前往放射腫瘤醫生處覆診預約非常重要。 他們會在覆診預約時檢查放射治療後的恢復情況。
在覆診預約前,請將問題和擔憂寫下來。 覆診預約時,請您帶同這張清單,以及一張列出您所有藥物的清單。 您也可以在放射治療結束後或在覆診預約之間的任何時間致電放射腫瘤醫生或護士。
在某些時候,放射腫瘤醫生可能會將照護您的工作轉交給一位倖存者執業護士 (SNP)。 這位倖存者執業護士 (SNP) 是 MSK 乳腺癌團隊成員。 他們與放射腫瘤學醫生密切合作。 隨着需求減少,您的倖存者執業護士 (SNP) 和放射腫瘤學醫生可能會將您的後續護理轉交給當地醫生。 轉交的時間將取決於您的特定癌症和治療計劃。
何時致電放射腫瘤學醫生或護士
如有以下情況,請致電放射腫瘤學醫生或護士:
- 發燒達至華氏 100.4 度(攝氏 38 度)或更高。
- 您有發冷情況。
- 皮膚疼痛、脫皮、起泡、濕潤或滲液。
- 您在受治療部位感到不適。
- 乳房、腋下或手臂變腫。
- 有任何新發或不尋常的症狀。
支援服務
MSK 支援服務
諮詢中心
www.msk.org/counseling
646-888-0200
很多人發現諮詢輔導服務能有所幫助。 我們的諮詢中心為個人、夫妻、家庭和團體提供輔導服務。 若您感到焦慮或沮喪,我們還可以開藥來幫助您。 請向您的保健提供者尋求轉介或撥打上述電話號碼,以進行預約。
綜合醫學與健康服務
www.msk.org/integrativemedicine
我們的綜合醫學與健康服務為患者提供多種服務,輔助(伴隨)傳統的醫療照護,包括音樂治療、身心療法、舞蹈及動作治療、瑜伽以及觸感治療。 請致電 646-449-1010,預約這些服務。
您還可以排期諮詢綜合醫學與健康服務的保健提供者。 他們將與您一起制定計劃以打造健康的生活方式,同時管理副作用。 請致電 646-608-8550 進行預約。
營養服務
www.msk.org/nutrition
212-639-7312
我們的臨床營養學家會透過我們的營養服務提供營養諮詢。 您的臨床營養學家將與您討論有關您飲食習慣的事宜。 他們還可就治療期間及其後的飲食提供建議。 請向您的照護團隊成員尋求轉介或撥打上述電話號碼,以進行預約。
復健服務
www.msk.org/rehabilitation
癌症及其治療或會使您的身體感到虛弱、僵硬或緊繃。 有些甚至會引起淋巴水腫(腫脹)。 我們的復健科醫師、職業治療師 (OT) 和物理治療師 (PT) 可以幫助您恢復日常活動。
- 復健科醫師會診斷和治療影響您移動及活動方式的問題。 他們能設計並幫助協調您在 MSK 或離家較近的地方進行復健治療計劃。如要了解更多資訊,請致電 646-888-1929 聯絡復健科醫師。
- 如您在日常活動上遇到困難,則職業治療師可以提供幫助。 例如,他們可以推介一些工具來使日常事務更為簡單。 物理治療師可以教您練習以增強力量和靈活度。 請致電 646-888-1900 聯絡復健治療,以了解更多資訊。
癌症治療後的生活資源 (RLAC) 計劃
646-888-8106
在 MSK,照護服務不會隨著治療結束而終止。 RLAC 計劃專為已完成治療的患者及其家人而設。
這個計劃有許多服務。 我們提供關於治療後生活的研討會、工作坊、支援小組和輔導服務。 我們還可以幫助解決保險和就業問題。
性健康計劃
癌症及其治療會影響您的性健康、生育能力或兩者皆有。 MSK 的性健康計劃可以在您的治療之前、期間或之後提供幫助。
- 我們的女性性醫學及女性健康計劃可協助解決過早絕經或生育等性健康問題。 請向您的 MSK 照護團隊成員尋求轉介或致電 646-888-5076,以了解更多資訊。
- 我們的男性性醫學及生殖醫學計劃可以幫助解決勃起功能障礙 (ED) 等性健康問題。 請向您的照護團隊成員尋求轉介或致電 646-888-6024,以了解更多資訊。
戒煙計劃
www.msk.org/tobacco
212-610-0507
MSK 有專家可以助您戒煙。 瀏覽我們的網站或致電上述號碼以了解更多資訊。 您也可以向護士查詢該計劃的詳情。
虛擬計劃
www.msk.org/vp
我們為患者及照顧者提供網上教育和支援。 這些是現場直播的環節,您可以交談或僅是聆聽。 您可以了解您的診斷情況、治療期間的預期情況,還有如何為您的癌症照護作準備。
相關環節由專家主持,屬私人性質,但費用全免。 瀏覽我們的網站以取得有關虛擬計劃的更多資訊或進行註冊。
放射治療支援服務
美國放射治療學和腫瘤學學會
www.rtanswers.org
800-962-7876
此網站提供了關於利用放射治療癌症的詳細資訊。 也提供了您所在地區的放射腫瘤醫生聯絡資料。
外部支援服務
在您接受癌症治療的前後和期間,有許多其他支援服務可以幫到您。 部分服務提供支援小組和資訊,而其他服務則可以助您解決交通、住宿(留宿地點)和治療費用等問題。
請細閱外部支援服務,以取得這些支援服務的清單。 您也可以致電 212-639-7020 以諮詢 MSK 社工。
可以問放射腫瘤醫生的問題
在應診前,寫下想要問的問題是很有幫助的。 詳情參閱以下例子。 應診時把答案記下,以便日後再次查閱。
我會接受甚麼種類的放射治療?
我會接受多少次放射治療?
接受放射治療期間,預計會出現甚麼副作用?
放射治療結束後,這些副作用會否消失?
完成放射治療後,預計會出現甚麼後期副作用?