This guide will help you and your loved ones understand what to expect throughout your chimeric antigen receptor (ky-MEER-ik AN-tih-jen reh-SEP-ter) T cell therapy. This treatment is most often called CAR T cell therapy.
This guide should not replace talking with your CAR T team. They’ll teach you about your treatment and what to expect. You can use this guide to help you remember. You can refer to it throughout your treatment.
We’ll explain some of the challenges you may have during your CAR T cell therapy and recovery. You may not face all of them. Try not to compare yourself to other people who had CAR T cell therapy. Everyone is different.
Overview
CAR T cell therapy is a type of immunotherapy (IH-myoo-noh-THAYR-uh-pee). Immunotherapy is a form of cancer treatment that uses your immune system to attack cancer cells. Different types of immunotherapy work in different ways, but they all help your immune system find and kill cancer cells.
You will get a CAR T cell infusion (in-FYOO-zhun) as part of your immunotherapy. An infusion is how we put the treatment into your bloodstream. This can be done safely whether you’re staying in the hospital (inpatient) or not staying in the hospital (outpatient). This guide has information about both inpatient and outpatient infusions. Your doctor will talk with you about whether an outpatient infusion is an option for you.
CAR T cell therapy is a long process. Getting ready for your infusion is just the first part.
- If you have an inpatient infusion: You’ll be admitted to the hospital some time right after your infusion.
- If you have an outpatient infusion: You and your caregivers will stay in an apartment near the hospital that’s approved by your doctor. Or, you’ll stay in a furnished apartment at MSK’s East 75th Street Patient Residence. You’ll visit the outpatient Cellular Immunotherapy Unit every day before, during, and for some time right after your infusion.
It’s normal to have many kinds of emotions during CAR T cell therapy. Your CAR T team includes social workers, chaplains (spiritual counselors), psychiatrists, and members of MSK’s Integrative Medicine Service. All these healthcare providers are here to support and help you and your caregivers cope with your feelings.
Communication is important
It’s very important to talk with your CAR T team and your caregiver about how you’re feeling physically and emotionally.
If anything is bothering you, even if it seems small, tell a member of your CAR T team. Do not wait and let things build up. That’s how small problems can become bigger problems. The more information you share with your CAR T team, the more they can help you.
Here are some ways you can communicate with your CAR T team.
By phone
Between and , call your doctor’s office. After , call 212-639-2000.
If you’re having an outpatient CAR T cell infusion, call the Cellular Immunotherapy Unit at 646-608-3150. A member of the team will answer. If a care team member is not available, your call will go to an after-hours telephone triage nurse.
In person
If you’re in the hospital:
Talk with any member of your care team. Ask to talk with your nurse, the charge nurse, clinical nurse specialist, or nurse leader. When you’re in the hospital (inpatient), it’s important to talk with your inpatient team, not the outpatient office.
You should also choose 1 caregiver to call the nursing station for updates. This person can share the updates with the rest of your friends and family. We’ll give you the nursing station phone number when you’re admitted to the hospital.
Through MSK MyChart
MSK MyChart (mskmychart.mskcc.org) is MSK’s patient portal. You can use it to check your appointment schedule, request a prescription refill, contact a healthcare provider, and find educational information.
How to enroll
Instructions for enrolling in MSK MyChart are printed on the bottom of your appointment print out. You can also read Communicating With Your Care Team: When to Call or Use MSK MyChart.
About PROMIS
Your CAR T team will use MSK MyChart to check in about how you’re feeling physically and mentally over time. They will send you a set of questions, called PROMIS. Your CAR T team will send PROMIS questions to your MSK MyChart account:
- On or near the day you start CAR T treatment.
- On the day of your CAR T cell infusion.
- Every 7 days for the first month after your CAR T cell infusion.
- Every month for the first year after your CAR T cell infusion.
- Every 3 months for the second year after your CAR T cell infusion.
There may be times you report concerning symptoms when you’re filling out the PROMIS questions. If so, you’ll either see a message asking you to call your care team, or they will call you to help.
Your answers also will help us know in general how people feel after CAR T cell therapy. This information helps us improve our care in the future.
How to use this guide
There’s a lot of information in this guide. Read the whole guide at least once, including the resources we include at the end. You may find it easier to read a few sections at a time, instead of all at once. We encourage you to refer to this guide throughout your treatment.
It’s a good idea to highlight or write notes on anything you do not understand or have a question about. There’s no such thing as a silly question. Please ask us about anything.
Medical terms
We have tried not to use many health terms that are hard to understand. Ask your healthcare provider about words or things you do not understand or search the National Cancer Institute (NCI) Dictionary of Cancer Terms.
Antigen and T cell basics
About antigens
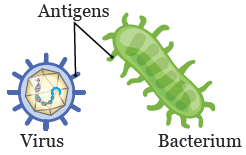
Antigens are substances (materials) that activate (turn on) your immune system. Your immune system helps your body fight infections and other diseases.
Antigens are on the surface of some things made inside your body, such as cells. They’re also on the surface of some things from outside your body, such as bacteria and viruses (see Figure 1).
About T cells
T cells help your immune system tell which antigens do not belong in your body. T cells are a type of white blood cell.
T cells have receptors that attach to certain antigens. Once a T cell attaches to an antigen, it sends messages to other cells in your immune system. These cells help kill the thing with the antigen and get it out of your body.
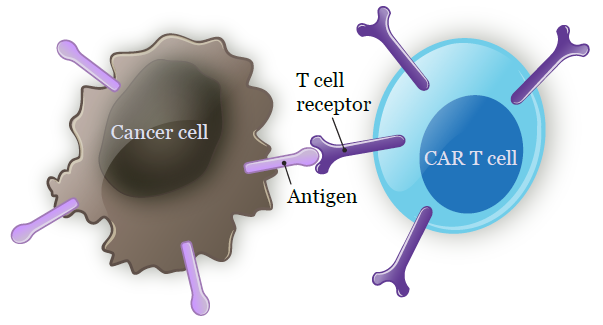
About chimeric antigen receptor (CAR) T cells
CAR T cells are T cells that were changed in a lab. They can now attach to antigens on cancer cells (see Figure 2). Once they attach, your immune system sends other types of immune cells to the cancer cells. The immune cells kill the cancer cell and get it out of your body.
Understanding your autologous CAR T cell therapy
Autologous (aw-TAH-luh-gus) means something taken from your own body, such as tissues or cells.
With autologous CAR T cell therapy, some of your T cells will be harvested (collected) from your blood. They’ll be sent to a lab to have a new gene added to them. This is called genetic modification (change). The new gene will help them find and kill cancer cells. Once the T cells have this new gene, they’re called CAR T cells.
Once the CAR T cells are made, you’ll get low doses of chemotherapy (chemo). This will help get your body ready so the CAR T cells can work as well as possible. The chemo is not meant to kill cancer cells.
When your body is ready, the CAR T cells will be infused (put) into your bloodstream.
Read the section “Phases of CAR T cell therapy” to learn more about what to expect.
Getting ready for your CAR T cell therapy
Your first consultation visit
During your initial (first) consultation visit, you’ll meet with your doctor and other members of your CAR T team. Your doctor will:
- Review your health and surgery history.
- Do a physical exam.
- Talk with you about what’s the best treatment plan for you.
They also may talk with other CAR T doctors to make sure everyone agrees it’s the best plan for you.
Blood Donor Room appointment
You’ll have an appointment in the Blood Donor Room. We will check if your veins are big enough to collect your T cells from a vein in your arm. If not, you will get a type of intravenous (IV) catheter called a leukapheresis (LOO-kuh-feh-REE-sis) catheter. We will use it for your T cell collection.
The donor room nurse will tell your care team if you need a leukapheresis catheter. If you do, your care team will give you more information. Read the section “Phase 1: T cell collection” to learn more.
Getting ready for your CAR T cell therapy
After your initial consultation visit, you’ll start making practical, physical, and emotional preparations for your CAR T cell infusion. Here’s a list of things that will happen and things you might need to do to get ready.
- Learn about your CAR T cell therapy. Your CAR T team will go over information with you. This is meant to help you learn, not scare you. Make a note of anything you do not understand or that is not clear. Ask questions.
- Choose a caregiver. Choose a family member or friend who can act as your caregiver. Make sure they understand what this role involves. Give your caregiver a copy of this guide and ask them to read it at least once. Read the section “Your caregiver” for more information.
-
Fill out a Health Care Proxy form. This form is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent. It can be a different person from your caregiver.
- To learn more about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn more about being a health care agent, read How to Be a Health Care Agent.
- Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
- Meet with a social worker. They will tell you about MSK’s psychological, emotional, and financial support services.
- Arrange for disability or a leave of absence from work. If you’re working, decide if you want to go on disability or take a leave of absence. Plan to be away from work for about 6 months. The exact length of time is different for everyone.
- Arrange for childcare and pet care, if needed. If you’re worried about talking with your children about your CAR T cell therapy, your social worker can help guide you.
- Have your pretreatment evaluation. You’ll have a few medical tests. Your clinical nurse coordinator will talk with you about which tests you need. Your doctor’s office coordinator will try to schedule these tests at a time that works well for you.
- Meet with a clinical dietitian nutritionist, if needed. They can help you with your nutrition needs and talk about your diet and safe food handling guidelines. If you want to meet with a clinical dietitian nutritionist, ask your nurse for a referral.
- Meet with a pharmacist. They’ll go over all the medicine you’ll take before and after your CAR T cell therapy.
Coping with being away from your children
During inpatient or outpatient CAR T cell infusions, you often spend more time away from your children than usual. Being away from your children may be hard for you and your family. We strongly recommend talking with your social worker about your concerns. Make a plan to keep strong ties to your children during your treatment.
Here are some things others have done to stay in contact with their children during their treatment.
- Talk with your children regularly using programs or apps like Zoom, Skype, Google Meet, or FaceTime. Set up a time you talk to them each day. This can be when they get home from school and before they go to bed. Get into a routine of using a computer, smartphone, or tablet to see and talk to them.
- Keep copies of your children’s favorite stories with you in your room. At night, you can use video chat to read along with them before they go to sleep.
- Use your cell phone or a tape recorder to record yourself reading your children’s favorite stories. Upload these recordings to the web, give them to your caregiver, or email them to your children. They can read along with the stories while listening to your voice.
- Decorate your hospital room with your children’s artwork and pictures of your family.
- Give your children a special coloring book or journal. They can use it when they miss you or are having trouble with their feelings. Your caregiver can bring their work to you. You can talk with your children about them over video chat or on the phone.
We know nothing will replace being able to hold your children. But we strongly encourage you to use technology to keep a strong bond with them while you’re away.
Your CAR T team
A large care team will work together to care for you during each phase of your CAR T cell therapy. You’ll meet many of the healthcare providers on your care team as you go through your CAR T cell therapy. You may not meet everyone, such as your doctor’s office coordinator, laboratory staff, or the CAR T cell service coordinator. But everyone on your care team is working to help you.
Here’s a list of your CAR T team members and their roles.
An attending doctor will be in charge of your care throughout your treatment. One doctor will be your primary (main) outpatient doctor, but different doctors may care you for while you’re in the hospital.
A fellow is a doctor who has finished general training and is getting more training in cancer care.
An advanced practice provider (APP) is a healthcare provider who works with your doctor to care for you. They can give medical treatments and prescribe medicine. Sometimes, you may see them instead of your doctor. APPs include nurse practitioners (NPs), physician assistants (PAs), and certified registered nurse anesthetists (CRNAs).
A clinical nurse coordinator is a nurse who works with you, your caregiver, and your team of doctors. They will organize and schedule testing, procedures, and consultations with other professionals you need before your infusion. Your clinical nurse coordinator will teach you about your treatment plan.
Nurses will work with you during your outpatient visits and while you’re in the hospital. They’re registered nurses (RNs) with special training in caring for people having stem cell transplants and CAR T cell therapy.
- Each outpatient nurse works with 1 or more attending doctors. You’ll meet your outpatient nurse during your initial consultation visit. Your outpatient nurse will see you at many of your outpatient visits after you’re discharged (leave the hospital). They will follow along with you during your CAR T cell therapy.
- You’ll have a team of primary nurses who will care for you during your treatment. They work 12-hour shifts. We will try to keep the same nurses working with you.
Both the inpatient and outpatient nurses work closely with your care team to manage your symptoms. They can help you with any questions or concerns.
A nursing assistant (NA) or patient care technician (PCT) works with your nursing team. They will help give you basic care and support, such as helping you shower.
A hospitalist is a doctor who sees people only while they’re in the hospital. At MSK, there’s a hospitalist on duty all night.
A clinical pharmacist is a pharmacist who works directly with you, your caregiver, and other members of your care team. They will review your medicines with you and your caregiver and teach you how to take them properly. They’ll also tell you about side effects they can cause. Your clinical pharmacists will have special training in caring for people having stem cell transplants and CAR T cell therapy.
A social worker helps you, your family, and friends manage the stress of going through CAR T cell therapy. Social workers understand the issues people having treatment face. They’re here to listen, offer counseling, and refer you or your loved ones to other resources and services.
A CAR T cell service coordinator works with you and your health insurer to learn about your treatment benefits. They know the insurance problems people face during CAR T cell therapy. Each health plan has its own policies and rules. When your insurer needs authorization, your CAR T cell service coordinator will help.
An office coordinator gives administrative support to your attending doctors and the nurses who work with them. You may talk with them to give us information, schedule an appointment, or have questions for your CAR T team.
A care coordinator works in an outpatient area. They track the flow of people in and out of the clinic. They make sure you schedule and complete all the tests, scans, and treatments your care team orders. Care coordinators also manage your health records and coordinate your future appointments.
A clinical research coordinator works with your care team. They’ll explain some of the research studies, also called clinical trials, you may be able to join. These studies mostly involve collecting samples or data.
A patient representative is the connection between you, your family, and MSK’s hospital staff. They’re here to protect your rights and help explain hospital policies and procedures. Patient representatives can help you with any concerns about your care. They can help you communicate with your CAR T team.
A clinical dietitian nutritionist is a food and nutrition expert. They’ll assess your nutritional health and talk with you and your caregiver about your diet. They will give you advice about changing your diet to help manage your symptoms and side effects.
A physical therapist (PT), occupational therapist (OT), or both will see you while you’re in the hospital. The PT will work with you to help you keep up your strength and stamina during your recovery. The OT will work with you to help you keep doing your daily activities.
A room service associate explains how room service works, including when it’s available and how to use it. They’ll make sure you get the right menus and deliver your meals.
A case manager will see you while you’re in the hospital. They’ll give your health insurer updates it needs to pay for your care. They’ll help you arrange home care, as needed.
Your caregiver
Choosing your caregiver is an important step in getting ready for your CAR T cell therapy. They will support you before, during, and after your infusion. Caregivers are usually a family member or close friend.
Your caregiver will be responsible for some of the medical, practical, and emotional support you will need.
Talk with your social worker if you want to hire a home health aide. They will give you information about these services.
For outpatient CAR T cell infusions
You must have a clear caregiver plan to have an outpatient CAR T cell infusion. There are no exceptions. Your CAR T team will talk with you about this.
Your caregiver must take you to and from your daily visits to the Cellular Immunotherapy Unit. They may not be able to work. They must stay with you for most of the day and night. Your caregiver can have some personal time while you’re in the Cellular Immunotherapy Unit for daily visits. We strongly recommend they take this time.
Your caregiver must be available 24 hours a day, 7 days a week during treatment and for some time after. The exact length of time you’ll need 24/7 caregiver support may vary. Your CAR T team will give them instructions about what they need to do. Here are some of the things your caregiver must do.
Medical support
- Get information from your CAR T team.
- Make sure you take your medicine.
- Keep a written record of when you take your medicine.
- Measure your temperature every 4 hours while you’re awake and away from the Cellular Immunotherapy Unit.
- Keep a written record of your temperatures.
- Keep a written record of how much you drink each day.
- Know how to take care of your central venous catheter (CVC).
- Notice any changes in your condition.
- Tell your CAR T team about any changes in your condition or new symptoms.
- Call for medical help in an emergency.
Practical support
- Take you to and from your daily appointments.
- Deal with financial and insurance issues.
- Handle food safely to prevent foodborne illness (food poisoning).
- Keep the place you’re staying clean.
- Keep family members and friends up to date about your condition.
- Manage how many visitors you have.
- Keep you away from anyone who’s sick.
Emotional support
- Pay attention to your moods and feelings.
- Communicate with you and listen to you.
- Understand your needs and your decisions.
- Feel comfortable contacting your care team if they’re worried about your emotional state.
The caregiver role for an outpatient CAR T cell infusion is full time, 24 hours a day, 7 days a week. It’s tiring, demanding, and stressful. That’s even more true if your condition, schedule, or treatment changes.
Your CAR T team will do everything they can to help your caregiver care for you. They can also refer your caregiver to other support services to help them manage their role.
For inpatient CAR T cell infusions
If you’ll be admitted to the hospital for your CAR T cell infusion. It’s important to have a caregiver plan for when you’re discharged from (leave) the hospital. We recommend you have a full-time, 24 hours a day, 7 days a week caregiver for the first 2 weeks after discharge. The exact length of time you’ll need 24/7 caregiver support can vary.
Your CAR T team will give your caregiver instructions about what they need to do. Here are some of the things your caregiver must do.
Medical support
- Make sure you take your medicine.
- Make sure you’re drinking enough and getting enough nutrients.
- Notice any changes in your condition.
- Call for medical help in an emergency.
Practical support
- Take you to and from your daily appointments.
- Deal with financial and insurance issues.
- Handle food safely to prevent foodborne illness (food poisoning).
- Keep the place you’re staying clean.
- Keep family members and friends up to date about your condition.
- Manage how many visitors you have.
- Keep you away from anyone who’s sick.
Emotional support
- Pay attention to your moods and feelings.
- Communicate with you and listen to you.
- Understand your needs and your decisions.
- Feel comfortable contacting your care team if they’re worried about your emotional state.
Choosing the right caregiver
Your caregiver must stay positive, calm, and flexible while giving you the support and encouragement you need. It’s also important for you to understand that the caregiver role is challenging. At times, your caregiver may feel overwhelmed by their role.
Take time now to think about who you want to be your caregiver. It should be someone you trust and who can take the time to care for you. Your caregiver should be someone who can give you the practical and emotional support you need.
If you do not have 1 person to be your caregiver, it’s OK to have more than 1 person share the role. It’s best to limit the number of caregivers to 1 or 2 people.
Resources for caregivers
Caregivers can have physical, emotional, spiritual, and financial distress. There are resources and support to help manage the many duties of caring for a person having CAR T cell therapy.
Contact your social worker for support resources and information. MSK’s Caregivers Clinic supports caregivers who are having a hard time coping with the demands of being a caregiver. Visit www.msk.org/caregivers or call 646-888-0200 to learn more.
Your pretreatment evaluation
Before you can have CAR T cell therapy, we will check your overall physical condition. This will help us make sure you’re ready for treatment. It will also help your CAR T team notice any changes later.
You’ll need to make a few trips to MSK to have tests. We often call this the work-up or restaging period. During the work-up, you must have some, but not always all, of these tests.
- Chest X-ray. This test confirms your lungs are clear and there’s no sign of infection or other problems.
- Blood tests. These are done to check a few things. This includes how well your kidneys and liver work, blood counts, and if you’ve been exposed to certain viruses.
- Urine test. This checks if there’s anything abnormal (not normal) in your urine (pee).
- Electrocardiogram (EKG) and echocardiogram (echo). These are done to give your CAR T team information about your heart.
- Pulmonary function tests (PFTs). These are breathing tests that measure how well your lungs work.
- Computed tomography (CT) scan. This is a radiology test that gives more detailed images of soft tissue and bone than a standard X-ray.
Sometimes, CT scans use contrast dye that you drink or have injected into your veins. It’s very important to tell your doctor if you know you have an allergy to contrast dye, seafood, or iodine. If you have a mild allergy, you can still have contrast dye. But you must take medicine before getting the dye so you do not have a reaction.
- Positron emission tomography (PET) scan. This is a radiology test that’s used to look at some types of cancer. It’s also used to look at your organs and how they work in your body.
- Brain magnetic resonance imaging (MRI) scan. This is done to look at your brain and how it works.
- Skeletal survey. This is done to see if cancer harmed your bones. It’s most often only done for people who have multiple myeloma. It involves taking X-rays of the major bones in your body. It can take a few hours.
- Bone marrow aspiration and biopsy. A bone marrow aspirate is a small sample of bone marrow. Most often, it’s taken from the back of your hip. Your doctor will numb your hip and place a needle into your bone marrow. They’ll take out a small amount of bone marrow.
Your doctor may do a bone marrow biopsy at the same time. This procedure collects a tiny piece of bone to examine. This is done to check how well your bone marrow is making cells. They will also look for any sign of cancer in the marrow.
These tests most often are done in the 30 days before your CAR T cell infusion (Day -30 onwards). Sometimes, the pretreatment evaluation can take longer.
Your CAR T team will work with you and your caregiver to schedule the tests. Your care team will use the results of the tests to plan your treatment. They’ll make sure it’s safe to start.
Your care team will explain any other tests you may need.
Your preadmission appointment
You’ll have your preadmission appointment after you finish your pretreatment evaluation and your CAR T cell infusion is scheduled. This appointment most often is 1 to 2 weeks before your scheduled CAR T cell infusion.
During this appointment:
- Your doctor will review your treatment plan with you. They will go over the consent forms. You’ll sign consent for your CAR T cell therapy, if you have not already signed it.
- Your clinical nurse coordinator will give you a calendar with your treatment plan. They’ll review the information with you and answer your questions.
- You’ll meet with your clinical pharmacist again. They’ll review the medicine you’ll take during and after your CAR T cell therapy.
We may ask you to sign a consent form for a transfusion, if you did not sign one already. You may need blood or platelet transfusions when your blood counts are low after your treatment. Read About Your Blood Transfusion.
You must stay healthy between your preadmission appointment and when you’re admitted to the hospital. It’s very important to call your CAR T cell doctor’s office if you have any of these things:
-
Signs of a cold, such as:
- A runny nose.
- Congestion.
- A cough.
- A fever of 100.4 °F (38.0 °C) or higher.
- Nausea (feeling like you’re going to throw up).
- Vomiting (throwing up).
- Diarrhea, which is loose or watery bowel movements (poop).
- A toothache.
- An open wound, such as a wound that’s bleeding or not healing.
- Any other new problem, even if it seems small.
Your healthcare provider will decide if we should delay your admission for CAR T cell therapy. It could be very dangerous to start your chemo while you have an infection, even if it’s just a cold. This is because your immune system will not be able to fight the infection.
Having your central venous catheter (CVC) placed
You’ll need a CVC during your CAR T cell therapy. A CVC is a catheter (thin, flexible tube) that’s put into one of your larger veins. Outside your body, the catheter divides into 2 or 3 smaller tubes called lumens.
A CVC lets your CAR T team infuse your CAR T cells and draw your blood. It also helps them give you fluids, electrolytes, blood transfusions, chemo, and other medicine. They will not have to keep sticking you with a needle. Having a CVC will make your treatment much more comfortable.
There are 2 main types of CVCs:
- A tunneled chest catheter is put into a large vein in your upper chest. Tunneled chest catheters are sometimes called Hickman catheters. Read About Your Tunneled Catheter to learn more.
- A peripherally inserted central catheter (PICC) is put into a large vein in your arm. Read About Your Peripherally Inserted Central Catheter (PICC) to learn more.
Your doctor or nurse will tell you which type of CVC you’ll have. CVCs are usually removed 2 to 3 weeks after your CAR T cell therapy is done.
What to expect in the hospital
This section has information about what to expect if you’re admitted to the hospital during any part of your treatment. Please read this section whether you’re having an inpatient or outpatient CAR T cell infusion.
While you’re in the hospital
There are a few units in the hospital that care for CAR T cell patients. The nurses on each unit have special training in caring for people having CAR T cell therapy. All the units follow the same guidelines.
You may need to change your room or floor while you’re in the hospital. We try to avoid this as much as possible. You may be in either a semi-private room or private room.
Your primary nursing team will care for you during your hospital stay.
Your nurses, patient care technicians, and nursing assistants most often work for 12-hour shifts. The shifts start at or When nursing shifts change, your nurse will update the nurse taking over. They’ll tell them anything they should know about you and your care during that shift.
The hospital environment
- Follow any instructions that are specific to your floor.
- Keep your hands clean. Read Hand Hygiene and Preventing Infection.
- Your room will have Wi-Fi and a TV with cable channels. You can also bring a streaming device to use on your TV. Amazon Fire TV Stick, Roku Streaming Stick, Google TV Streamer, and Apple TV are examples of streaming devices.
- You’ll be connected to an IV pole with electronic pumps during most of your hospital stay. Disconnecting from the IV pole often can raise your risk for a CVC infection. It’s important to keep your IV pole connected during your stay.
- If you’re at risk for falling, someone will help you get to the bathroom. Your healthcare team will tell you more about how to keep from falling while you’re in the hospital. You can also read Call! Don't Fall!.
Testing and evaluations
- A member of your care team will weigh you and take a sample of your blood before 6 a.m. each day. They will check to see how your white blood cells, red blood cells, and platelets are recovering.
- We will do other blood tests as needed. These tests check how well your kidneys and liver work and check for infections. The tests tell us the level of chemo or other medicine in your blood. This information helps your care team assess your overall condition.
- Your care team will check your vital signs every 4 hours, even during the night. This includes your blood pressure, heart rate, breathing, and pain level.
- Your care team will give you medicine during your stay. Please do not bring any of your own medicine to the hospital.
- Your care team will measure your urine throughout the day. It’s important that we know how much urine you’re making. They will also ask you how much water or liquids you’re drinking.
- You’ll have tests to check your neurological (brain) function. Your nurse may ask you simple questions.
Visitors
-
Your family and friends are welcome to visit you. You must not have any visitors who:
- Have symptoms of an illness, such as a cough, rash, fever, or diarrhea.
- Think they may be getting sick.
- May have recently been exposed to someone with an infectious (contagious) illness.
- All visitors must always clean their hands before entering your room.
- Visitors and caregivers must use the visitor’s restroom in the hallway, not the restroom in your room. This is to limit the spread of bacteria in your room.
- You are not allowed to have fresh, dried, or live flowers or plants in your room. Please tell your family and friends not to bring or send them.
- Children aged 12 and under cannot visit some inpatient floors, including M7 and M8.
Exercise
You’ll feel tired after your chemo and CAR T cell infusion. But you should still try to stay active and get out of bed each day. It’s important to be safe, so ask for help when you get up.
We encourage you to walk around the unit. You may need to wear a mask and gloves while you’re walking around. Your nurse will tell you if you also need to wear an isolation gown. Do not leave the floor when you’re walking or exercising.
Soon after you’re in the hospital, you’ll meet with a physical therapist. They’ll prescribe an exercise program that’s right for you.
Communication
Each room has a call bell system that’s monitored 24 hours a day, 7 days a week. If you need something, use your call bell. Tell us what you need so we can send the right member of your care team member to help.
Diet
Your CAR T team will plan your diet. They will give you a menu and instructions for ordering your meals. A room service associate will deliver your meals to you.
If you keep kosher, have diabetes, or follow another special diet, tell your clinical dietitian nutritionist. We will prepare your meals properly. Your clinical dietitian nutritionist is also here to help you plan your meals.
Showering
You’ll be expected to shower daily. A patient care technician or nursing assistant will be in your room when you’re showering. They’ll help you and make sure you’re safe.
Mouth care
It’s important to take good care of your mouth. This will help reduce infections and mouth sores. Your nurse will go over this with you. You can also read Mouth Care During Your Cancer Treatment for more information.
What to expect in the Cellular Immunotherapy Unit
During an outpatient CAR T cell infusion, you’ll get most or all your care in the Cellular Immunotherapy Unit. You’ll visit the unit every day. We’ll only admit you to the hospital if you need more care than we can give you as an outpatient.
What to bring to the Cellular Immunotherapy Unit
When you come to unit every day, bring the following:
- A list of all prescription and nonprescription medicines you’re taking, their dosages, and how often you take them. This should include patches, creams, vitamins, nutritional supplements, herbal products, and over-the-counter medicines. An over-the-counter medicine is one you can buy without a prescription.
- All the prescription medicines you were told to take during your CAR T cell therapy.
- Your Outpatient Cellular Therapy Temperature & Liquid Intake Log. Your caregiver will use this to keep track of your temperature and liquid intake while you’re away from the unit.
- Things to pass the time, such as books, newspapers, an audio player, a laptop, or tablet. Do not forget the charger for your electronic items.
- A notebook to write down information and any questions you or your caregiver have.
While you’re in the Cellular Immunotherapy Unit
Please arrive at your scheduled time.
Wear comfortable clothing. Wear clothing that makes it easy to access your CVC. This can be a shirt that opens in the front, a sweatshirt, or a large T-shirt. Do not wear clothing that’s hard to take off or put back on.
After you arrive
After you check in, a member of your care team will bring you to a room. They will:
- Check your vital signs and weight.
- Ask you about any symptoms you have.
- Check your blood counts, electrolyte levels, and kidney function (how well your kidneys are working).
Then, you’ll wait in your room for your test results to be ready. This can take a few hours. You’ll have an entertainment unit with a TV and computer to pass the time. You can also bring food and snacks with you.
This is a good time for your caregiver to take a break, take some personal time, or run errands. You’ll be safe in your treatment team’s care. We highly recommend your caregiver leaves the hospital and takes this time to relax.
Planning your care
Your CAR T team will plan your care after they get the results from your blood tests (sometimes called labs). The rest of your visit that day will depend on your test results. Based on your test results:
- Your healthcare provider may give you fluids through your CVC.
- Your healthcare provider may give you an infusion of platelets, red blood cells, or other blood components.
- Your healthcare provider may change some of your medicines.
- Your treatment could be left as is.
You’ll stay in the unit until you finish your treatments. After that, your caregiver will take you to where you’re staying. There, they’ll monitor your temperature and how much you drink.
Read About Your Appointments in MSK’s Cellular Immunotherapy Unit to learn more.
What to do in your home or apartment
Your caregiver will take care of you when you’re not in the Cellular Immunotherapy Unit.
We will give you a printed copy of these resources, or you can find them online. Keep them out in your home or apartment so you and your caregiver can get them easily.
- Outpatient Cellular Therapy Temperature & Liquid Intake Log
- Outpatient Cellular Therapy Emergency Guide (Color)
Carry your Outpatient Cellular Therapy Emergency Card with you
If you’re having an outpatient CAR T cell infusion, you’ll get an Outpatient Cellular Therapy Emergency Card (Wallet Card - Color). Keep this card with you at all times. It has important information about who to call and where to go if you have a medical emergency.
If you need emergency medical care, show this card to the medical professional helping you.
Keep track of how much you drink
Drink 2 liters (64 ounces) of liquids every day. Try to drink small amounts throughout the day. Your caregiver must keep track of all the liquids you drink in the Outpatient Cellular Therapy Temperature & Liquid Intake Log.
Keep track of your temperature
From the time you start getting your chemo, your caregiver must take your temperature every 4 hours while you’re awake. We will give you a thermometer.
If you have a fever of 100.4 °F (38 °C) or higher, your caregiver needs to take you to Urgent Care Center as instructed in your Outpatient Cellular Therapy Emergency Guide (Color).
Call the Cellular Immunotherapy Unit at 646-608-3150 while you’re on your way there.
Check for bleeding
Always tell someone from your CAR T team if you have any bleeding. If you notice you’re bleeding and you’re not in the Cellular Immunotherapy Unit, follow these steps right away:
- Put pressure directly on the bleeding site. If you’re bleeding from your nose, also put ice over the bridge of your nose.
- Follow the instructions in your Outpatient Cellular Therapy Emergency Guide. Call the Cellular Immunotherapy Unit at 646-608-3150. Your care team will give you more instructions based on the type of CAR T cell you get.
Call your doctor right away if you have any of these while you’re not in clinic:
- Black bowel movements (poop), blood in your bowel movements, or bleeding from your anus.
- Blood in your urine (pee).
- A headache that does not get better.
- Blurred vision.
- Dizziness.
- Coughing up or vomiting blood.
- A nosebleed that does not stop after putting pressure or ice for a few minutes.
Move around and exercise
You’ll feel tired after your chemo and CAR T cell infusion, but you should still try to stay active. A physical therapist will talk with you and prescribe an exercise program that’s right for you.
To learn more about why it’s important to stay active and what your care team can do to help, read Staying Active During Stem Cell Transplant.
Phases of CAR T cell therapy
There are 6 phases of CAR T cell therapy. The following table gives a summary of each phase. Keep reading for more information about each of the phases.
| Phase | Description |
|---|---|
| Phase 1: T cell collection | We collect some of your T cells from your blood. Then, we send them to a lab to be genetically modified (changed) into CAR T cells. This will help them recognize and kill cancer cells. This step is done about 4 to 6 weeks before your infusion. It takes about 2 to 4 hours. |
| Phase 2: T cell modification | While your T cells are being genetically modified into CAR T cells, you’ll have your pretreatment evaluation and pretreatment testing. You’ll also use this time to finish planning for your CAR T cell infusion and recovery. You may also get other treatment during this time. This will help control the cancer before your CAR T cell treatment starts. T cell modification takes about 3 to 4 weeks. |
| Phase 3: Lymphodepleting chemotherapy (conditioning) | Once your CAR T cells arrive at MSK, you’ll get lymphodepleting chemo. This chemo will help the CAR T cells work better at finding and killing cancer. You will get lymphodepleting chemo about 3 days before your infusion. Your CAR T team will tell you how long it will take. |
| Phase 4: CAR T cell infusion | Your CAR T cells will be infused into your bloodstream through an IV. This may be done in the Cellular Immunotherapy Unit or the hospital. CAR T cell infusion takes about 5 to 30 minutes. |
| Phase 5: Early recovery | You’ll have appointments daily or every few days. Your CAR T team will see how you’re doing and manage your side effects. You’ll stay in the hospital or nearby. Early recovery lasts for about 4 weeks after your infusion. |
| Phase 6: Long-term recovery | You’ll have appointments every few weeks or months. Your CAR T team will see how you’re doing and manage your side effects. You’ll come back to MSK for these appointments. You may be coming from another hospital. If so, you may be seen by the doctor who referred (sent) you to MSK between your visits to MSK. Long-term recovery lasts for about 100 days or longer after your infusion. |
Phase 1: T cell collection
Your T cells will be collected in MSK’s Blood Donor Room. It will take about 2 to 4 hours.
Before your T cell collection
Have a leukapheresis catheter placed, if needed
If you need a leukapheresis catheter, it will be placed 1 to 2 days before your collection. Your nurse will tell you what to expect. You can also read About Your Tunneled Catheter.
The leukapheresis catheter will be put into a large vein in your upper chest. It’s most often removed a few hours after your collection.
Eat foods high in calcium
For 1 to 2 days before your collection, eat dairy products and other foods that are high in calcium. You should also bring a high-calcium snack to eat during your collection. This can help keep the level of calcium in your blood from getting too low during your collection. Your nurse will give you a list of foods that are high in calcium.
During your T cell collection
Your collection will be done while you’re on a bed or in a recliner chair. If you want to, you can watch TV or read during your procedure. You may feel cold during the procedure. We will give you blankets to make you comfortable.
Some of your blood will be collected from your bloodstream through an IV line or leukapheresis catheter. The blood will flow through a machine that filters out the T cells and other white blood cells. The rest of your blood will be given back to you through another IV line.
Your donor room nurse will watch for side effects. They will give you medicine as needed. If you feel numbness or tingling in your fingertips or around your mouth, tell your donor room nurse. These are signs your calcium level is low. Your donor room nurse can give you calcium tablets to help.
After your T cell collection
If you had an IV line in your arm: Your donor room nurse will take it out. They’ll apply a bandage to prevent bleeding. They’ll tell you when you can take the bandage off.
If you’re still bleeding after you take the bandage off, put gentle, firm pressure on the site for 3 to 5 minutes. Call your doctor if the bleeding does not stop.
If you had a leukapheresis catheter: Your donor room nurse will schedule an appointment to take it out soon after your collection.
Most people can go back to doing their regular activities right after their T cell collection.
Phase 2: T cell modification
After your T cells are collected, they’ll be sent to a lab to have a new gene added to them. This is called genetic modification (change). The new gene will help them find and kill cancer cells. Once the T cells have this new gene, they’re called CAR T cells.
Your CAR T cells will be ready about 3 to 4 weeks after your collection.
While your T cells are being modified, you’ll complete your pretreatment evaluation and preadmission testing. You may also have chemo to control the cancer.
This is also a good time to finish planning for your CAR T cell therapy. It’s very important to make sure you’ve made plans for where you’ll stay. You also must choose your caregiver. Read the sections “Getting ready for your CAR T cell therapy” and “Your caregiver” for more information.
Phase 3: Lymphodepleting chemotherapy (conditioning)
Once your CAR T cells arrive at MSK, you’ll get chemotherapy to help get your body ready for the CAR T cell infusion. This is called lymphodepleting chemotherapy. Lymphodepletion is the process of lowering your white blood cell numbers with chemotherapy. It’s done to help get your body ready for the CAR T cells.
Most people get their lymphodepleting chemotherapy in the Cellular Immunotherapy Unit. It’s usually done a few days before the CAR T cell infusion. Your clinical nurse coordinator will give you your schedule and talk with you about what to expect. Your schedule depends on your specific medications and treatment.
Phase 4: CAR T cell infusion
If you’re having an inpatient CAR T cell infusion: You’ll be admitted to the hospital. This most often happens the day before your infusion. Your infusion will take place in your hospital room.
If you’re having an outpatient CAR T cell infusion: Your infusion will take place at the Cellular Immunotherapy Unit.
Before your CAR T cell infusion
The day of your CAR T cell infusion, you’ll have a general check-up and neurologic tests. You’ll also get medicine to help keep you from having a reaction to the infusion. If you do not have a CVC, you’ll get an IV line placed in 1 of your veins.
Your CAR T team will tell you what time you can expect to get the infusion.
During your CAR T cell infusion
Your healthcare provider will give you the CAR T cell infusion through your CVC or IV line. The infusion can take 5 to 30 minutes, depending on your treatment plan. A staff member will be in the room with you for at least the first 15 minutes of your infusion. They’ll probably stay with you for the entire infusion.
After your CAR T cell infusion
We will watch you closely for side effects. Cytokine release syndrome (CRS) and neurological changes are common side effects of a CAR T cell infusion. CRS is a group of symptoms that happen when T cells attack cancer cells.
Common symptoms of CRS include:
- A fever of 100.4 °F (38 °C) or higher
-
Flu-like symptoms, such as:
- Muscle aches
- Headaches
- Chills
- Feeling very tired
- Nausea
- Vomiting
- A faster heart rate than usual
- Feeling dizzy or lightheaded
Common neurologic changes include:
- Confusion
- Trouble finding words
- Tremors
- Seizures (shaking you cannot control)
- Sleeping more than usual
- Feeling very drowsy and responding more slowly than usual
Not everyone gets the same type of CAR T cell therapy. Everyone does not respond the same to each type of therapy.
These side effects will go away. Your care team will watch you carefully for side effects. They’ll manage any side effects. It’s very important you or your caregiver tell your care team if you may be having any of these side effects.
Phase 5: Early recovery
The first 4 weeks after your CAR T cell infusion are considered the early recovery phase.
Early recovery after inpatient CAR T cell infusion
If you had an inpatient CAR T cell infusion, you’ll stay in the hospital for 1 to 2 weeks or longer after your infusion. How long you stay in the hospital depends on how your body reacts to the cells.
Your CAR T team will care for you and keep watching for side effects. Some side effects need to be watched more closely and may result in you moving to the Intensive Care Unit (ICU).
Once you’re ready, you’ll be discharged from the hospital. If you live more than 2 hours from MSK, you’ll stay in an apartment near the hospital or at MSK’s 75th Street Patient Residence.
Before you leave the hospital, your CAR T team will give you discharge instructions. Here are some guidelines to follow:
-
Call your CAR T team if you have:
- A fever of 100.4 °F (38.0 °C) or higher
- Chills
- Confusion
- Hallucinations (seeing or hearing things that are not there)
- Headaches
- Seizures
- Dizziness or lightheadedness
- Trouble breathing
- Bleeding
- Faster heart rate than usual
- Severe nausea, vomiting, or diarrhea
- Pain
- Any other changes in condition
- Do not drive for 8 weeks or until your care team says it’s OK to.
- Carry your wallet card with you at all times. Show it if you go to the emergency room, urgent care, hospital, or when you see a doctor.
- If you go home with your CVC or PICC, your nurse will teach you how to care for it at home.
- Avoid family and friends that may be sick.
Early recovery after outpatient CAR T cell infusion
If you had an outpatient CAR T cell infusion, you’ll have daily appointments for the first 2 weeks after your infusion. Your appointments will be at the Cellular Immunotherapy Unit. During your visits, your CAR T team will check how you’re doing and help manage any side effects you’re having. You’ll be admitted to the hospital if needed.
Starting about 2 weeks after your infusion, you may be able to have appointments less often. This depends on how you’re feeling. Side effects are still common during this time, so it’s important to come to all your scheduled appointments.
About 4 weeks after your CAR T cell infusion, you’ll start having your appointments in your doctor’s regular clinic instead of the Cellular Immunotherapy Unit.
Phase 6: Long term recovery
Long term recovery is different for everyone. It depends on your situation and how the cancer reacts to your CAR T cell therapy. Your CAR T team will tell you what to expect.
You’ll have appointments with your CAR T team about 30 days, 100 days, and 1 year after your CAR T cell infusion. During these appointments, you’ll have tests to check how you’re doing. These tests might include:
- A physical exam.
- Blood tests.
- Imaging scans, such as a PET scan or CT scan.
- Bone marrow aspiration and biopsy.
Your CAR T team will use the results of these tests to plan your care during your recovery.
Your CAR T team will talk with you about going back to seeing your primary doctor during your long term follow-up. If you do start seeing your primary doctor, please be sure to update your CAR T team on how you’re doing.
Some people need to come back to the CAR T team for more care. This may include being seen in the outpatient clinic or being admitted to the hospital.
Educational resources
This section lists the educational resources mentioned in this guide and some other resources that may be helpful.
You can find these resources online or you can ask for a printed copy. You can also search for more educational materials on the Patient and Caregiver Education website, www.msk.org/pe
- About Your Appointments in MSK’s Cellular Immunotherapy Unit
- About Your Blood Transfusion
- About Your Peripherally Inserted Central Catheter (PICC)
- About Your Tunneled Catheter
- Advance Care Planning for People With Cancer and Their Loved Ones
- Building Your Family After Cancer Treatment: For People Born With Testicles
- Building Your Family After Cancer Treatment: For People Born With Ovaries and a Uterus
- Call! Don't Fall!
- Communicating With Your Care Team: When to Call or Use MSK MyChart
- Fertility Preservation Before Cancer Treatment: Options for People Born with Ovaries and a Uterus
- Food Safety During Cancer Treatment
- Hand Hygiene and Preventing Infection
- Improving Your Vulvovaginal Health
- Mouth Care During Your Cancer Treatment
- Outpatient Cellular Therapy Emergency Guide (Color)
- Outpatient Cellular Therapy Temperature & Liquid Intake Log
- Sex and Your Cancer Treatment
- Sexual Health and Intimacy
- Sperm Banking
- Staying Active During Stem Cell Transplant