Nine students will don caps and gowns to celebrate their academic achievements and receive their PhDs from the Gerstner Sloan Kettering Graduate School of Biomedical Sciences (GSK). The degrees will be awarded on May 30 during GSK’s seventh commencement ceremony at Memorial Sloan Kettering’s 39th academic convocation.
This year’s degree recipients are Kinisha Gala, Jens Hamann, Catherine Konopacki, Danilo Macalinao, Gregory Mazo, Brandon Nemieboka, Joseph Pucella, Piero Sanfilippo, and Neel Shah. Their graduation brings the total number of GSK alumni to 53.
“Students benefit from our school’s renowned faculty, innovative curriculum, and interactive environment that features a close integration of basic science, clinical research, and patient care,” says GSK Dean Kenneth Marians. “We are proud of our graduates and their extraordinary work, which exemplifies these cornerstones of the GSK experience.”
As PhD candidates, the students successfully defended their dissertations over the course of the past year. Their research, summarized below, reflects GSK’s mission to prepare its students to work in research areas related to human disease, particularly cancer.
Kinisha Gala

Ms. Gala completed her thesis work under the guidance of physician-scientist Sarat Chandarlapaty. Dr. Chandarlapaty’s research focuses on the regulation of growth factor–signaling networks in cancer. His lab, which is part of MSK’s Human Oncology and Pathogenesis Program, is particularly interested in the causes of resistance to targeted therapies for breast cancer.
Ms. Gala’s dissertation centered on one mechanism that breast cancer cells may use to escape the effects of certain targeted drugs. She studied estrogen receptor–positive (ER+) breast cancer cells that rely on the activity of the estrogen receptor for growth. Her findings showed that ER+ breast cancer cells that have mutations in the epigenetic factor KMT2C were resistant to hormone therapies that specifically target the estrogen receptor. She also found that KMT2C is an important regulator of estrogen receptor activity.
“These findings are important as we continue to better understand estrogen receptor regulation and develop second-line therapies to treat drug-resistant tumors,” says Ms. Gala, who was a Grayer Fellow in 2014.
Ms. Gala is thankful for the invaluable experience she acquired in Dr. Chandarlapaty’s lab. “My wonderful colleagues and brilliant mentor helped me build on this brand-new project in the lab, and I was able to hone my basic science skills while gaining exposure to both translational and clinical research,” she says. “I could not have asked for a more student-focused, supportive school.” Ms. Gala has begun a postdoctoral fellowship in the Department of Pediatrics at the University of California, Los Angeles.
Jens Hamann

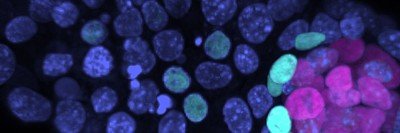
Mr. Hamann completed his dissertation research under the mentorship of cell biologist Michael Overholtzer. Dr. Overholtzer’s lab studies the mechanisms of tumor initiation and progression, cell adhesion, and cell death. Mr. Hamann’s work centered on cell death pathways, which are frequently deregulated in cancer. He endeavored to understand how cells respond to changes in critical nutrients, such as amino acids and sugars, in order to survive.
Solid tumors often experience metabolic stress because they don’t get a sufficient supply of nutrients through the body’s existing network of blood vessels. As a result, these cancer cells must develop new ways to obtain the molecular building blocks they need.
Mr. Hamann found that cells can cannibalize neighboring cells in response to glucose starvation. This process, called entosis, allows the starving cells to degrade and kill weaker surrounding cells in order to survive. He also identified that a protein called AMPK, which activates in cells in response to energetic crisis, causes certain cells within tumor cell populations to be ingested by their neighbors.
Mr. Hamann showed that glucose starvation selects for the cannibalistic cells and that engaging in entosis enables them to survive and proliferate. He also demonstrated that the DNA content of the surviving cells is altered, suggesting that they may develop genetic mutations that could make them more likely to promote tumor growth.
“These findings reveal a new way for tumor cells to acquire nutrients in order to prolong survival during metabolic stress,” says Mr. Hamann. “Future studies are needed to further address the role of entosis in cancer.”
Mr. Hamann, who was a Grayer Fellow in 2014, is now a postdoctoral associate at Weill Cornell Medical College.
Kasia Konopacki
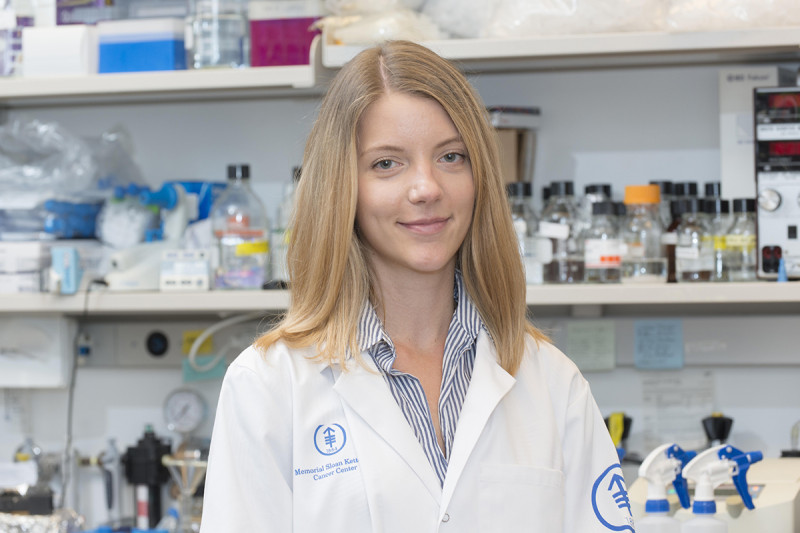
Ms. Konopacki, who was voted by her peers to be the student speaker at this year’s commencement, completed her thesis work in the laboratory of Alexander Rudensky, Chair of the Immunology Program at the Sloan Kettering Institute and Director of the Ludwig Center for Cancer Immunotherapy at MSK. She chose to study a subset of immune cells called regulatory T (Treg) cells in the context of breast cancer.
Treg cells help rein in immune responses once they are no longer needed, preventing an attack on the body’s healthy tissues. It is a function called autoimmunity. Although essential to maintaining order, Treg cells also impede the immune system from attacking tumors effectively.
To identify features unique to Treg cells in cancer, Ms. Konopacki characterized Treg cells in healthy tissue and compared them to Treg cells that accumulate in breast tumors. While she found very few differences between tissue-resident and tumor-resident Treg cells, there was one cell-surface protein, CCR8, that was highly expressed on tumor-resident Treg cells in breast cancer, colorectal cancer, and lung cancer.
“Research is ongoing to develop an antibody against CCR8 that will specifically deplete the tumor-resident Treg cells while maintaining Treg cell presence in the rest of the body,” Ms. Konopacki notes.
“GSK was an incredible place to pursue my doctorate on a topic that I am passionate about,” she says. “My experience in Dr. Rudensky’s lab helped me develop my research and project management skills and taught me how to think critically, solve complex problems, and communicate effectively to a wide range of audiences.” Ms. Konopacki is currently exploring opportunities within the life sciences.
Danilo Macalinao

Mr. Macalinao completed his dissertation research in the laboratory of Joan Massagué, Director of the Sloan Kettering Institute. Dr. Massagué’s lab studies the control of stem cell growth and phenotypes in tumor progression, metastasis, and response to therapy.
Cancer metastasis occurs when cells break off from a tumor, spread through the bloodstream or lymph vessels, and establish themselves in another part of the body. Metastasis accounts for the majority of cancer deaths and can develop many years after the initial diagnosis and treatment of the primary tumor.
Metastatic latency describes a state in which cancer cells are able to remain dormant for an extended period of time before eventually emerging to form overt disease. Mr. Macalinao’s work explored mechanisms of metastatic latency and outgrowth in HER2-positive (HER2+) breast cancer. People with HER2+ disease who are treated with HER2-targeted therapies are susceptible to developing metastases — often in the brain — after a protracted period of being disease free.
Mr. Macalinao developed new models for understanding metastatic latency and outgrowth in the brain. He observed that cancer cells that underwent metastatic latency were able to evade the immune system, notably natural killer cells. He also found that cancer cells that spread to the brain conditioned the environment around them by secreting prometastatic proteins that facilitated their progression.
“Collectively, these findings shed light on how HER2+ cancer cells might be able to stay latent for long periods of time in host organs and clarify the traits that these cells need in order to exit from latency and initiate metastatic outgrowth,” says Mr. Macalinao, who was named the Robert B. Catell Fellow in 2012.
Mr. Macalinao is now working toward a masters of divinity at Catholic University in Washington, DC, where he entered the seminary with the Paulist Fathers, a community of Catholic priests who serve North America.
Gregory Mazo

Mr. Mazo carried out his thesis work in the laboratory of cell biologist Meng-Fu Bryan Tsou. Dr. Tsou’s lab studies how mammalian cells produce, maintain, and operate their primary cilia. Cilia are hairlike organelles that are normally located on the surface of a cell and function as antennas to sense a variety of signals. Some cilia-mediated signaling pathways, especially the sonic hedgehog pathway, are misregulated in multiple types of cancers. A clear understanding of these cilia antennas is therefore relevant to human disease.
Cilia antennas are thought to function only at the cell surface. However, many vertebrate cells choose to form submerged cilia that are confined inside a deep membrane pit and appear not to be ideal for signaling. How and why cells change or control the location of their primary cilia has long been a mystery.
A cylinder-like organelle called the centriole is known to function as the template that drives cilia formation. Mr. Mazo found that structures at the sides of the centrioles called subdistal appendages help keep the cilia submerged in cooperation with another structure located at the proximal end of centrioles. Simultaneous loss of all these structures allows submerged cilia to fully surface and respond to stimuli. The difference in physical and biochemical properties between surfaced and submerged cilia suggests that they are functionally distinct.
“No cilia position phenotype had ever been reported before, so this work represents important progress in the understanding of cilia position,” says Mr. Mazo. “More research is needed to determine whether a surfaced cilia position enhances signaling and whether cilia in certain cancers are surfaced or submerged.”
Mr. Mazo received the Chairman’s Prize for his work in 2017 and the Geoffrey Beene Graduate Student Fellowship in 2011. He is currently a research fellow in the lab of physician-scientist Liang Deng at MSK.
Brandon Nemieboka

Mr. Nemieboka enrolled in GSK as a student in the Tri-Institutional MD-PhD program, which trains physician-scientists to become leaders in biomedical research. It is collectively sponsored by the Sloan Kettering Institute, The Rockefeller University, and Weill Cornell Medical College.
Mr. Nemieboka conducted his doctoral work in the laboratory of radiochemist Jason Lewis. Dr. Lewis’s research focuses on the development of molecular imaging agents for the diagnosis and treatment of cancer.
Mr. Nemieboka is specifically interested in ovarian cancer. It is the most lethal gynecologic cancer and the fifth leading cause of cancer-related deaths in women in the United States. As of 2015, the five-year survival rate for advanced-stage ovarian cancer was 27 percent. This is largely because four out of five women with ovarian cancer are diagnosed with advanced disease that has spread throughout the abdominal cavity.
“Advances across a variety of fields are needed to improve the clinical management of this disease, which claims the lives of more than 14,000 women in the United States each year,” notes Mr. Nemieboka. His dissertation centered on the introduction of molecular imaging strategies, specifically PET imaging, for earlier diagnosis and management of ovarian cancer.
He studied two transmembrane proteins, MUC16 and L1CAM, which are highly overexpressed in ovarian cancer. He discovered that specific modifications to the Fc region of monoclonal antibodies can dramatically alter their bio-distribution profile in mouse models.
“Using this information, we designed antibodies targeting MUC16 and L1CAM that can potentially be used with PET imaging for the diagnosis and treatment of ovarian cancer,” says Mr. Nemieboka. He is now completing his MD degree at Weill Cornell Medical College.
Joseph Pucella

Mr. Pucella conducted his dissertation research in the laboratory of immunologist Jayanta Chaudhuri. Dr. Chaudhuri studies the mechanisms of immunoglobulin gene diversification.
B cells are a type of white blood cell, or lymphocyte, that forms the basis for effective vaccine protocols. In response to immunization, they become activated and mature into cells that produce antibody proteins, which are necessary to fight off infection. However, this process can be dangerous because activated B cells proliferate and acquire DNA mutations that make them prone to transforming into cancerous lymphoma cells. For these reasons, engaging B cells during an immune response must be tightly regulated.
Mr. Pucella sought to uncover novel regulatory roles in humoral or antibody-driven immunity for a class of small nucleic acids called microRNAs. He found that a microRNA called miR-182 regulates B cells as they mature in response to immunization. However, he demonstrated in a mouse model that miR-182 is not essential to adaptive or acquired immunity. “In an intriguing turn of events, this work contradicted previously published studies and pointed to the likelihood that the data generated may need to be reassessed,” Mr. Pucella noted.
He further cemented his work by studying humoral responses in a second mouse model in which miR-182 was deleted together with related microRNAs in the miR-182 family. In doing so, he ruled out an interpretation of his earlier results by disproving the suggestion that miR-182 family members compensated for the loss of miR-182 itself.
“This work is important because it underscores a vital need to reevaluate what we know about microRNAs and fuels the debate surrounding the characteristics of microRNA interaction networks in physiology,” says Mr. Pucella, who was selected as the Olayan Fellow in 2011. Mr. Pucella has begun a postdoctoral position at New York University School of Medicine.
Piero Sanfilippo
Mr. Sanfilippo completed his graduate studies in the laboratory of developmental biologist Eric Lai. Dr. Lai studies diverse regulatory networks in cell patterning and behavior. Mr. Sanfilippo’s research sought to better understand the complex role of regulatory elements called 3’ UTRs in messenger RNA, the key molecule that makes the DNA-encoded information of a gene available to the cell to make cellular building blocks called proteins.
The information encoded in 3’ UTRs regulates key aspects of protein synthesis, such as its levels, timing, and location. Recent advances in sequencing technologies have uncovered that the same gene can give rise to messages with different 3’ UTR lengths. Mr. Sanfilippo’s work characterizes this novel phenomenon in the fruit fly Drosophila melanogaster.
Mr. Sanfilippo generated a comprehensive genomewide atlas of 3’ UTR variants in Drosophila melanogaster. He uncovered that the vast majority of genes in the fruit fly give rise to multiple messenger RNA variants that differ in 3’ UTR length. He also found specific patterns of 3’ UTR variant expression in neural and ovary tissues and identified evolutionary signatures that shed light on the mechanism that gives rise to the expression of specific 3’ UTR variants.
In addition, Mr. Sanfilippo wanted to better understand the functional role of a specific class of 3’ UTRs, which are extremely long and expressed in the nervous system. He discovered that the messenger RNA of the gene Elav is expressed in all tissues, contrary to the neural-specific expression of the Elav protein. He went on to identify microRNA regulators that are directly involved in inhibiting Elav protein expression outside of the nervous system by acting through the 3’ UTR.
“This work demonstrates an unanticipated role of 3’ UTRs in mediating tissue-specific patterns of protein expression by inhibiting protein expression outside of a desired domain,” observes Mr. Sanfilippo. “The findings illustrate the functional role that these regulatory elements can play in biology.”
Mr. Sanfilippo received a Geoffrey Beene Graduate Student Fellowship in 2010.
He is currently pursuing postdoctoral research at University of California, Los Angeles, where he is investigating the role that neurotransmitter receptors play in the wiring of the nervous system.
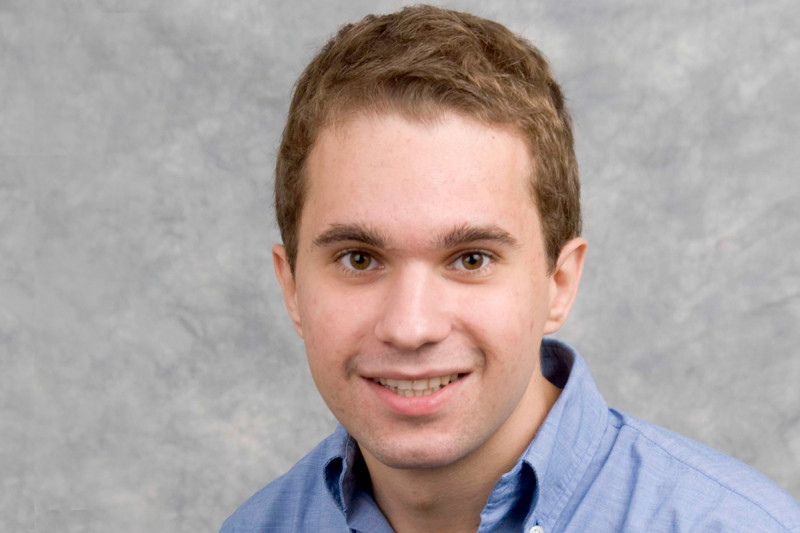
Neel Shah
Mr. Shah completed his dissertation work under the mentorship of Charles Sawyers, Chair of the Human Oncology and Pathogenesis Program. Dr. Sawyers’s laboratory is investigating signaling pathways that drive the growth of cancer cells, with an eye toward designing molecularly targeted cancer treatments.
Mr. Shah’s thesis research elucidated new mechanisms of resistance to hormone therapies in the treatment of advanced prostate cancer. While men with metastatic prostate cancer initially respond well to hormone therapies such as antiandrogens, they invariably progress to a lethal stage of the disease termed castration-resistant prostate cancer (CRPC). It is largely unknown why this occurs.
Using preclinical models of CRPC, Mr. Shah helped discover that upregulation, or higher expression, of the glucocorticoid receptor (GR) is an important mechanism of resistance to the antiandrogen drug enzalutamide (Xtandi®). GR, which is a hormone receptor that helps regulate genes involved in cell development, metabolism, and immune response, is able to bypass the need for direct androgen-mediated signaling in prostate tumor growth.
He also determined that GR is epigenetically regulated in the progression of prostate cancer and that it is reactivated through a tissue-specific enhancer in CPRC. Mr. Shah further observed that GR expression could be targeted in resistant tumors using a novel class of drugs called BET bromodomain inhibitors, which effectively resensitize the tumors to enzalutamide treatment.
“Overall, these findings not only reveal an underlying mechanism of drug resistance but also suggest a novel treatment strategy to target a specific subset of prostate tumors,” says Mr. Shah, who received a Geoffrey Beene Graduate Student Fellowship in 2012. He is now a research fellow at the Dana-Farber Cancer Institute.